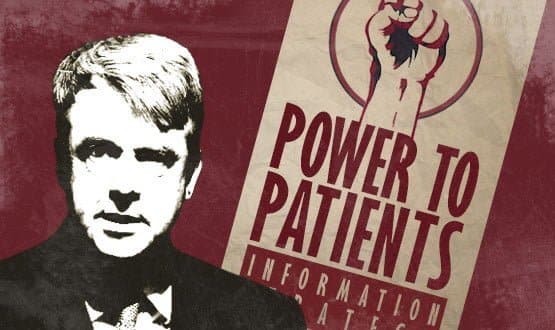
The seventh Earl Howe is an unlikely revolutionary, yet he hopes his department’s new information strategy – ‘The Power of Information’ – will set in train a far-reaching upheaval in the way healthcare services are delivered.
The parliamentary under secretary of state, who has a background in banking, says the strategy is “deliberately bold and consciously so.”
It is intended to create a culture shift among health professionals and patients that will enable a “digital first” NHS to be built from the ground up over the next decade.
In an exclusive interview with eHealth Insider, the minister said the strategy is framed to set the ambition of a digital health service, which promises to be as transformative as the information revolutions that have re-shaped other sectors.
“Our task is to give a sense to patients and the public of how transformative this technology can be to their own lives.”
The strategy also aims to catalyse action by providing “a series of ideas on how this could be done, and already is in places being achieved.” But it is not intended to prescribe how the health services, or individual organisations, should get there.
Quality underpinned by information
A key theme in the strategy is for the government to step back and create the conditions that will enable quality information, local innovation and best practice to flourish and spread only intervening where necessary. Or as Earl Howe put it: “The role of the centre is to facilitate the process.”
The role of the centre is to set the direction of travel and create the conditions for local innovation, together with core infrastructure “including standards.” Use of the NHS Number and pushing adoption of SNOMED CT are the two mentioned by the strategy.
Power to the patient
Like health secretary Andrew Lansley, Earl Howe spent a long period as a shadow health spokesperson, first taking up the job back in 2004, and becoming a health minister with responsibility for quality in 2010.
He told EHI that information absolutely underpins the quality agenda and Lansley’s commitment to “no decision about me without me.”
He added: “It’s about the empowering clinicians to make better decisions and allowing patients to see their information, to order prescription refills, book appointments or to have a remote consultation with their doctor.”
These digital services will not replace face-to-face services, but supplement them and help precious consultation time to be more effective and efficient.
“We have to be careful we don’t give the impression that digital services are a substitute for face-to-face services,” said Earl Howe, adding that “digital first” does not mean digital for all.
“There are many patients and service users who will either not be able to, or who will not want to, access digital services.”
Asked whether he anticipated financial incentives to GPs would need to be required to stimulate e-consultations in particular, the minister said: “We will have to talk to the respective leaders for GPs about whether financial incentives are necessary or effective. I don’t rule that out.”
He added: “I would like to think the case sells itself to GPs. All the evidence we have from France, Denmark and Sweden shows that it’s a much more effective use of resources.”
Promoting patient access
One of the few, firm commitments in the strategy is to give patients online access to GP records by 2015. Earl Howe said most system suppliers already provided the capability, “but only 1% of practices so far use it.”
He also said work is underway with the Royal College of General Practitioners to agree guidelines on patient access to records and that, as an interim step, the DH will publish details of which practices offer record access by 2013.
“We will be publishing information on which practices have and have not delivered on that promise.”
The minister told EHI that his own GP doesn’t yet offer online access to records, although he offers online appointments. “I’ll make sure he does soon,” he joked.
Overall, the aim is to create a cultural shift among patients so they come to use information to “take much greater control of their health and well-being.”
Earl Howe said he’d recently seen a particularly powerful demonstration; a service that used a patient portal to provide patients with COPD and asthma with highly targeted information on local services, and even the weather.
However, he said that a similarly ambitious cultural change is needed among clinicians, social care professionals, managers and information experts.
CCIOs ‘an ideal model’ for leading clinical change
The minister said he strongly backed the chief clinical information officer role as a model of how to create local clinical leaders. “It is certainly, in my view, an ideal model to have a CCIO. To appoint someone with that title and role sends a very strong message.”
Money’s too tight to mention?
The new information strategy has little to say on money, and Earl Howe said this was again deliberate. “We are no longer going to award large national contracts and will be moving to a much more local approach from 2016, as the National Programme [for IT in the NHS] contracts come to an end.
“The balance of funding and decision making will become much more local.” It will be down to provider organisations and local commissioners to deliver the strategy. “We’re confident that funds earmarked for local commissioning will be utilised by CCGs [clinical commissioning groups].”
Asked about the over-hang of NPfIT, the minister said: “I am the first to say that NPfIT has delivered some major benefits. What has not yet happened, and what needs to be changed, is to deliver the local systems we are talking about in this strategy.”
On next steps the strategy says that a series of implementation plans will follow. But no separate technology strategy is being worked on, as was once mooted.
Earl Howe said that it will be the responsibility of the NHS Commissioning Board and Public Health England to oversee implementation across health and social care.