Last week, Digital Health News attended the King’s Fund Digital Health and Care Congress in central London, where professionals from the healthcare landscape came together to address the progress and challenges in bringing digital into the clinical toolkit.
On the first day of the event, King’s Fund researchers presented some of the key findings from their latest report, ‘Digital change in health and social care’. The report stressed the importance of tight-knit collaboration in bringing large-scale technological initiatives to fruition: not just between providers and suppliers, but across entire organisations.
King’s Fund analyst and report co-author David Maguire offered that digital transformation should not be seen an IT change, but instead as “a clinical change that uses technology”.
Meanwhile, fellow co-author Matt Honeyman said that the culture gap between technology and clinical needed to be overcome so that the desire to change could “reach across a spectrum of attitudes and bridge cultures” within organisations.
Reflecting on digitisation efforts at Royal Liverpool and Broadgreen University Hospitals, chief executive Aidan Keho argued that technology was the only means by which the NHS would be able to face “long-term pressures” facing the healthcare system.
“In the years ahead, we are going to need digital technology and solutions much more,” said Keho.
“We are dealing with more and more complex patients coming through door and we have a massive workforce crisis…international recruitment is not going to solve this.”
Transformation projects will test friendships
A later session explored lessons learnt from national and regional NHS digital transformation projects.
Hosting the session was Andy Fenton, associate director of digital transformation at NHS South Central and West CSU.
Fenton noted that while there had been “fantastic examples” of technology being used to improve care pathways, the “huge amount of diversity” between data-sharing initiatives raised the question of how this data could be brought together.
He also advised that large-scale projects “puts very strong challenges around partnership working” and “really test out the boundaries of collaborative work”.
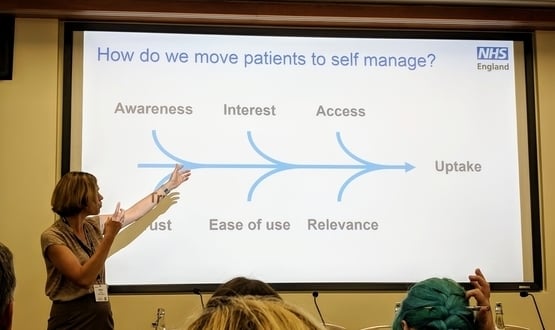
Providing all patients will equal access to digital healthcare technologies was another stand-out theme from the event on 10 June, and was visited during a session exploring how implementation and adoption of patient-facing digital tools could be accelerated.
Polly Bishop, head of digital strategy and engagement at NHS England, suggested that primary care practice was “an obvious place to engage” with people.
Bishop added that being able to physically demonstrate new technology to patients helped to this end.
“If you’ve got something on your phone you can show people, it just makes life easier,” she added.
“The best way to learn about it and see the benefits is do it for yourself.”
No ‘postcode lottery’ for digital health
Bishop further argued that key to driving the adoption of digital health services like online GP consolations was providing equal access to all patients regardless of where they were located.
“We should be a position where wherever we are in England, we do not have a ‘postcode lottery’ for digital access to health and care services.”
“We need to widen digital participation…people who lack digital skills would benefit most from them. It’s important we think about that.”