Industry Spotlight: Alan Payne, group product and engineering director, the Access Group
- 22 May 2024
Alan Payne, group product and engineering director with the Access Group, tells Jennifer Trueland that unleashing the potential of community and third sector services is key to reducing friction in the system and improving outcomes for patients
When Alan Payne joined the health sector after a first career in banking, he couldn’t quite believe how primitive the digital landscape was. But now, some two decades later, he believes a sea change is finally happening.
This is great for patients, he says, and for those who work in the health and care system, but it’s also potentially transformative for the wider population.
He is a strong believer in the value of prevention – of stopping bad health before it happens or mitigating it at an early stage – and says that sharing information is vital for making the shift from a health service that reacts, to one that is proactive, and which enables people to be cared for in the best place for them.
Learning the lessons from other sectors, including banking, has been a key part of this journey.
Know your customer
“The whole ethos of banking in the 1990s to early 2000s was around efficiency of process and knowing your customer,” he says. “It’s a big change going from banking to healthcare, but what I saw was that there were none of the things that had been sorted out in banking 25 years previously, like a single view of the customer. Is there a single view of the patient? No, there isn’t, and when you go into a doctor’s office you can still see the brown files coded in mysterious hieroglyphics.
“But if you look at things that make a difference, it’s about information sharing – which is exactly what banking is – knowing your customer, being able to risk manage that person, exactly as a doctor, or a nurse, or social worker would manage that risk.
“I’ve really spent the last 20 years or so of my career refining banking principles to scaling healthcare interoperability and understanding the patient.”
Payne admits that when he joined the health sector, he didn’t think this necessary transformation would take as long as it has, and that the sometimes glacial progress can be frustrating. “There are so many vested interests. Governments change every four years, and it’s only fairly recently that the Government [in England] has actually started creating integrated care boards. That joins funding pools together so you can look at the preventative agenda, and the social care agenda, aligned with the healthcare agenda – which has always been predominant and the senior partner in the equation – which is positive. But it didn’t go far enough.”
Vital role of community services
He would like to see community services and the third sector integrated into this new landscape, believing that they have a vital – and often unrecognised – role to play both in keeping people healthy and improving outcomes and quality of life when they do live with ill health.
Creating a truly frictionless system, where primary, secondary, social care, community and the third sector work together would help to dissolve blockages that create financial and capacity woes for the NHS, while benefiting patients and families.
“You’ve got this thing called community care that sort of sits in the middle – domiciliary care, nursing homes, care homes, community centres, the power of the third sector (particularly with social prescribing) and the ability to start removing the need for additional demand on an already broken system. You cannot supply, in the current methodology, the number of people needed to deliver care – that’s why we’ve got five-year waiting lists, it’s why you have delayed discharge, it’s why you have social care that’s still arguably in the 1980s. It’s not because of a lack of quality people; it’s just the processes and barriers that sit within silos.”
Community care is the linchpin that sits between health and social care, he adds, but the whole system needs to work more smoothly.
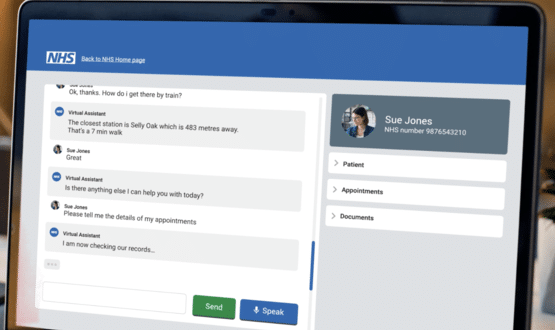
He uses the analogy of Airbnb, where people seeking accommodation can put their requirements into a digital system that will match them to suitable places to stay, based on factors such as preferred location and whether dogs are allowed. “It’s the same for a patient who is in hospital but doesn’t need to be there. You want to be able to put the criteria in, so that it comes back with the best alternatives based on your criteria. If you can digitise it, like Airbnb has, you can match resources to take people where they need to be, with what they need to be there, whether that’s equipment, or a reminder to take their vital signs themselves if they’re capable, or if not, we can send a nurse or a carer in.
“By using the power of community care, you start to remove a lot of friction, costs, and associated pressure, and you don’t end up with issues where patients are sent 200 miles away from their nearest family member because that’s the only place they can find.”
Imaginative social prescribing
Being more imaginative about how to keep people well and socially connected is also key to keeping them living well at home, he adds – and social prescribing is an important element of that. He gives the example of Merseyside where Access’s social prescribing solution is used by GPs to suggest non-drug approaches such as social interaction to patients who present with particular conditions or circumstances. “We’ve linked that into GP systems so that when a certain drug comes up, it will suggest prescribing an activity instead.”
Funding systems and the current culture in health and care remain the major challenges, he says, but not tackling them is short-sighted. “The funding models are so geared towards reactive care. In the UK, we’ve got one of the best reactive care systems in the world – if you’re going to get really sick, this isn’t a bad place to do it. But if you want to think about preventing people from actually getting sick, that’s where we’re not so good.”
Payne was tempted to move to Access – although he was contemplating early retirement – because it aligned with his values and his long-held vision. “I wrote my first paper on virtual wards in 2013,” he says almost ruefully. “For me, creating integrated care at scale has been a lifelong ambition. And that’s something we’re offering our customers.”
Contact the Access Group:
Website: www.accessgroup.com
X (formerly Twitter) @theaccessgroup
Linkedin: The Access Group