It is early Friday morning at Central Manchester University Hospitals NHS Foundation Trust, but in the trust’s informatics department, the day has already begun.
The trust does as much IT development as it can in-house, and has a lot on its plate as it prepares to go live with an electronic patient record system developed entirely by its informatics team.
This means there are many issues that need to be addressed, and what better way to do so than at the weekly EPR breakfast club?
Apart from the informatics team, those present include the trust’s deputy head of nursing and the head of quality improvement, as well as Manchester’s recently appointed technology partner, Kelway.
Working in-house
“Many our clinical systems have been developed by our staff,” says Helen Ainsbury, the trust’s director of informatics. “We need to be frugal about how we spend money. Doing developments in-house is not as high in cost as going with a third party supplier."
Ainsbury adds that internal developments can also be quicker than going out to procurement, and that it is easier to secure clinical engagement with them.
“What we’re saying is that everything we do as a third party procurement, we will counter-tender and do internally as well,” she further explains.
“It’s what we’re doing for maternity and we’re also going to do it for e-prescribing,” she says, adding that the trust will probably do the same for its patient administration system replacement.
“There’s no reason why we shouldn’t be able to do it,” she says matter-of-factly, as she takes a sip of her coffee.
The fact that these are massive tasks, which would seem very daunting to most trusts, does not seem to faze her or anyone else around the table.
Admittedly, the trust does have a very large IT team, with 20 software innovation developers, six integration developers, and seven business intelligence developers, to mention just part of the team.
Hundreds of systems, one view
Richard Adams, the trust’s head of software innovation, explains that doing things on their own is nothing new to the trust.
“Over the last three years we’ve developed 20 systems, including for nursing ward rounds, ward management and children’s mental health,” he says.
Still, with more than 700 systems running within the trust, it is impossible to replace all of them in-house, so some, smaller specialist systems, will have to be supplied by a third party. However, they will be integrated within a new EPR, known as Chameleon.
“Ideally, we want to bring these 768 systems together under one cohesive view of a patient. We are building our clinical portal at the moment, which has single sign-on, also done in house; but it’s a challenge getting access to all these systems,” says Adams.
Focusing on design and usability
The trust is due to go live with the Chameleon next month. The system will give clinicians a beautifully designed system the trust is very proud of. Adams compares its usability with services such as Facebook or eBay.
“Very few people need training to use Facebook. They should be able to use [NHS IT] intuitively, and that is the approach we take in developing our systems,” he says.
“We employ one person who just focuses on the usability,” Ainsbury says. “I’ve seen so many EPRs that look awful, but Chameleon doesn’t.”
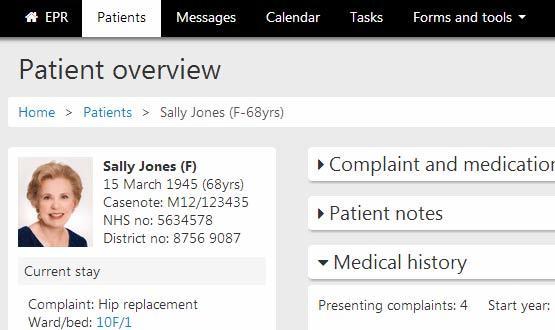
The EPR shows a list of patients under the specific clinician’s care, so they know how they are responsible for. For each patient, there is a task list of what needs to be done, and who that task has been assigned to.
Chameleon, which also has a tablet view, then gives clinicians a patient overview, demographics, needs assessments, a slideshow of the patient’s x-rays, medical history, allergies and alerts. At the moment, Adams explains, some information is read-only, due to restrictions with other systems.
DIY PAS?
Like many other trusts, Central Manchester was affected by the failure of the National Programme for IT. The trust worked towards getting Lorenzo, the iSoft/CSC EPR that was slated to be the ‘strategic’ system for the North, Midlands and East for many years.
But, in the end, it left the programme shortly before it was dismantled. “We have got a Clinicom PAS, which is ancient and still on green screen,” Ainsbury says. On the other hand, she says replacing it is not an immediate priority because “it works.”
“Eventually we’re going to replace it in-house but we need to replace it in sections. We’re going to phase out the information gradually until there’s nothing left of it,” she says.
The trust, which runs five hospitals as well as several community sites, is taking a similarly phased approach to the Chameleon go-live. At the end of November, it will begin with two wards at Manchester Royal Eye Hospital, before gradually moving on to the rest of the trust.
Lovely whiteboards
IT having a positive impact on healthcare is not all about big systems, though. On the Clinical Decision Unit at Manchester Royal Infirmary, ward manager Anya Dykins, is less concerned about the future EPR and more concerned with her shiny touch screen whiteboards, of which the ward has three.
The ward is one of 14 that have already implemented the whiteboards across the hospital, with another 19 to go before Christmas. “It’s really pretty, isn’t it,” she says, quite smitten.
The electronic whiteboard updates automatically if someone adds information to the electronic nursing handover system. Alternatively, they can simply touch the screen and change the details; although Dykins has yet to master that.
“There is something wrong with my fingers; it takes a few taps for me to get it. But it’s brilliant,” she says, adding that the best thing is that it saves people from coming up and asking “where is so and so”?
“We get a lot less interruption,” she says. “It’s just a quick glance of where the patients are and their status. Everyone can now just come up to the board and see what’s going on.”
Lisa Elliott, the trust’s quality improvement manager, and former nurse, says the whiteboards, which are specialised for each ward, are very popular.
“We just can’t roll it out quick enough, everyone is so keen to get it,” she says. Small changes make a big difference.”
Thinking about the community
Changes are also being made to the trust’s community services. Central Manchester recently took over Trafford Healthcare NHS Trust and its community services and has decided that overall, community needs a bit of an IT upgrade.
School nurses and health visitors were given laptops last year, and the trust is due to go live with a cloud based network in its 40 community sites later this month.
“We start the roll out of the cloud in October, and by March all the sites will be on the cloud. We have 1,500 mobile devices and we want to make sure the devices have full functionality,” Ainsbury says.
“We expect the cloud infrastructure for the first two sites to be in place by mid-October, and then fully operational for community users with connectivity and new devices by end of October.”