UCLPartners launches how-to guide for setting up virtual NHS clinics
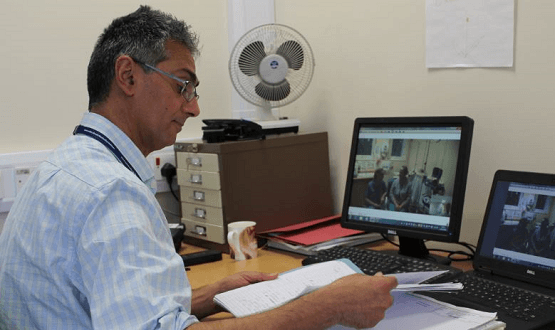
UCLPartners has launched a free online guide for NHS managers and clinicians on setting up virtual clinics.
The new how-to guide, developed in collaboration with NHS clinicians, managers and patients, provides a comprehensive guide to setting up non-face-to-face clinics, including how to develop a project plan and business case.
The guide is delivered through both text and videos and can be accessed via UCLPartners website.
Virtual clinics are viewed as crucial for reducing unnecessary outpatient visits, saving time and money for patients and the health service.
The NHS aims to avoid up to a third of face-to-face outpatient visits over five years, removing the need for up to 30 million outpatient appointments each year.
However, to date there is little practical guidance on how to develop this approach, according to UCLPartners.
Steve Shaw, medical director for outpatient transformation for NHS London said: “We know that the current model we have for provision of outpatients is not working as well as it should in London. We need to improve the experience for both patients and staff.
“Non face-to-face clinics can help reduce unnecessary visits to hospitals but are still a relatively new model of care. This comprehensive guide is a welcome resource to help teams develop and embed this approach.”
[themify_box icon=”info” color=”gray”]
Partners involved in developing the resource include:
- Barts Health NHS Trust
- Royal Free London NHS Foundation Trust
- University College London Hospitals NHS Foundation Trust
- Whittington Health NHS Trust
- University College London
- North Middlesex University Hospital NHS Trust
- One London
- Queen Mary University of London
- Patient and public representatives
[/themify_box]
A number of NHS trusts and GP practices already make use of virtual clinics, most of which target outpatient appointments.
Despite this – and NHS targets to improve access to digital GP services – a survey by the Royal College of Physicians found that just one in 10 doctors had recently conducted outpatient appointments via video.
This had led to calls to provide more digital training to GPs in order to help them prepare for the NHS’s digital-first service requirements, though a perceived lack of funding for digital initiatives has cast uncertainty over NHS targets.
‘Two models’ of virtual clinics
UCLPartners defines virtual clinics as being deliverable through two models: ‘synchronous’, where patients and clinicians interact in real time, for example by webcam or phone; and ‘asynchronous’, where patients and clinicians interact at different times.
One example of this would be when secondary care specialists make decisions about a patient’s management based on data gathered in primary care.
Professor Mike Roberts, UCLPartners Managing Director and a respiratory physician, said: “NHS outpatient visits to hospitals have doubled in the past decade. This guide – based on the experiences and insights of our NHS partners and patients – provides practical support to those looking to set up non-face-to-face clinics, with benefits for patients and staff.”
Patients can also benefit from digital GP appointments as it reduces the need to travel and take time off of work and out of their their social lives.
Raj Mehta, patient and public representative for the project, said: “I believe delivering outpatient care in a non face-to-face model provides many benefits, such as easier to access care, reducing travel costs, costs for parking, childcare, time off work and increasing choice for patients.
“As patients, we have contributed to this resource as we’re all passionate about making a difference to the current way that outpatient care is delivered to better suit the needs of patients, public and clinicians.”
UCLPartners’ guide can be accessed here. The group will be hosting a launch event for the guide on 11 February.




