Maidstone and Tunbridge Wells NHS Trust has halved its bed turnaround time using a centrally managed patient tracking solution.
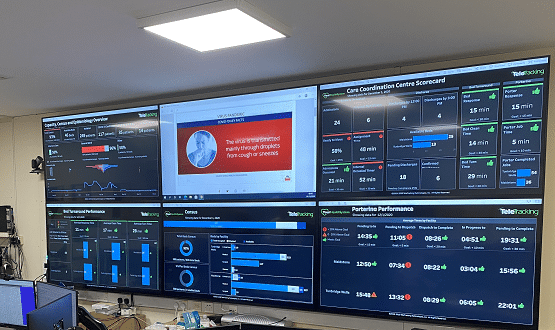
The trust implemented a Care Co-ordination Centre last year to gain better oversight of where patients were moving in the hospital, which beds are free and which beds require cleaning before a patient can be admitted.
The centre operates across the trust’s two sites – Maidstone Hospital and Tunbridge Wells Hospital – and provides real-time visibility of beds. Since it went live on 24 November 2020, the centre has halved bed turnaround times- from around 150 minutes to 60 minutes on average.
It has also reduced the number of hours patients are waiting in the emergency department by 110 hours per day due to the reduced time it takes to get a patient from the emergency department into a clean bed – down from an hour and a half about 30 minutes in each hospital.
Nick Sinclair, director of operations at the trust, said the solution allowed the trust to move away from a “pencils and rubbers” way of tracking patients.
Sinclair spent 21 years working in ambulance trusts and said he was “used to technology dispatching ambulances and paramedic crews to the right place at the right time”.
“I was thinking ‘there has to be a better way’, how do we digitalise our bed management. I started my research and came across TeleTracking and we headed in that direction,” he told Digital Health News.
The contact for the Care Co-ordination, powered by TeleTracking’s patient flow platform, was signed in June 2020, with a go-live planned 20 weeks later.
“What it does is it takes real-time information from our two hospital sites and gives our clinical site managers visibility of all our beds and their status – is a patient in them, is that bed empty and ready to be occupied by the next patient or is it empty and waiting to be cleaned?,” Sinclair said.
“On the other side of it we have the real time view of the patients who are waiting for those beds, whether they are from the theatre, the emergency departments or any planned admissions.
“It allows them [clinical managers] to best manage our capacity so our patients get access to a bed as quickly as possible when they need one.”
From contract signing to go-live
The trust was able to implement the solution in 22 weeks due to the technical aspects being “fairly straightforward”.
When asked the advice he has for other trusts looking to implement similar bed management systems, Sinclair said culture is usually the biggest obstacle.
“The bit that we really have to work on is changing culture, and changing hearts and minds on how the organisation is going to operate, because it’s a massive change going from a manual way of operating to this,” he said.
“Getting all of the people who need to be onboard and using the system understanding why they’re doing it is the bit that you really need to focus on.”
Part of the work to introduce the new system included a “complete redesign” of the way the clinical ward managers and porters work, Sinclair added.
The platform integrates with the trust’s Allscripts patient administration system (PAS) which makes it easier for the systems to share patient information, such as location, with clinical teams.
Porters are notified of patients being allocated a bed via iPhone, they can then update information on the Care Co-ordination platform when the patient is in the right bed.
Alongside that, wards have been fitted out with large touchscreen displays that allow nurses and clinical staff to update the system once patients are moved to different areas of the hospital, or when beds become available.
By using a digital-first way of operating it’s given hospital staff “complete oversite” of patients and beds which “truly allows you to choose the right bed for the patient first time”, Sinclair said.
“One of the main benefits is we have complete oversight. In order to manage your capacity effectively you need to know what’s coming in, what you’ve got and which patients are leaving,” he added.
“The time that is saves… and it allows our nursing teams to concentrate on providing care because they’re not answering telephones being asked about how many beds they’ve got and who is going home, that’s all marked on the system very quickly by the ward teams.”
Elective backlog
As the NHS recovers from the Covid-19 pandemic it faces another wave of pressure from the backlog of elective surgeries postponed due to the crisis.
Sinclair believes bed management systems like the one in place at Maidstone and Tunbridge Wells will play an important role in managing an influx of surgeries. According to Sinclair the trust is the highest performing trust in Kent when it comes to elective surgeries, which he said would not have been possible without the Care Co-ordination Centre.
“The period we’re going through at the moment, with that elective backlog of patients that have been waiting months… the quicker that we can turn that around the better, he told Digital Health News.
“Since the introduction of Care Co-ordination we’ve got much better oversight of our elective activity coming in, so it allows us to balance our beds better because we know what’s coming.
“Previously you would have missed the odd elective case on lists from a bed management point of view, but now we have overall visibility of everything that’s coming into the trust.”
Next steps
Sinclair hopes the trust will be able to build up from the Care Co-ordination Centre to expand it across more of the hospital’s sites. TeleTracking provides a theatre module for the system that would allow clinical teams to better manage patients through theatre.
The supplier has also developed a nursing app, which Sinclair hopes to adopt across the trust in the coming months. The app will “give nurses real-time information within the bay area on whichever device they happen to have”, he added.
Eventually, Sinclair aims to have the Care Co-ordination Centre as the single point of contact for the trust, giving complete oversight of patients from NHS 111 referrals right through to discharge.
Alongside with on the Care Co-ordination Centre, the trust is in the process of deploying the Sunrise electronic patient record (EPR) from Allscripts, which works alongside the PAS.
It is aiming for a go-live date in October, before starting work on an electronic prescribing and medicines administration (EPMA) module.