Advisory Series: Mobile and modern working
- 22 August 2017


Mobile and modern working –
Advisory Series, August 2017

By Claire Read – Digital Health
When considering the benefits of mobile working in the healthcare, the focus has often been on clinical staff working in the community. But mobile technology is also being valuably used to improve care within hospital walls and to help non-clinical staff work more efficiently, as Claire Read reports.
To welcome the concept of mobile working in a healthcare organisation is often to welcome a whole load of preconceptions along with it. Chief among them, according to James Reed, is the overly-simplistic idea that healthcare didn’t previously have a way of working in such a fashion.
“When you have hard copy notes, you’ve sort of got mobile working,” points out the chief clinical information officer at Birmingham and Solihull Mental Health NHS Foundation Trust. “OK, the notes are only in one place [at once], but when you have big trusts you often end up with multiple sets of notes, so the individual staff member can sort of do mobile working.
“So when you put electronic systems in, what you actually do initially is you cut all that off, because you say to people, well, you can’t take the notes with you anymore, because they’re all on the computer.”
An initial barrier
It was, he says, a barrier to be overcome when the trust implemented its RiO electronic patient record back in 2011. Enabling mobile working quickly became central to the organisation’s information technology strategy, and it remains so – a section in the trust’s successful global digital exemplar bid was dedicated to the topic.
In detailing how he’d like to see mobile working develop at the organisation in the coming years, Reed dispenses with another preconception: that such means of working are of most value to staff who are based in the community.
Yes, he speaks of a desire to expand existing on-the-go access to RiO for staff who primarily work outside of hospital walls. That might also include “the more logistical things – so you know where all the job bands are, and you know roughly when they’re going to get from one place to the next”.
Into inpatients
But he also sees huge potential in the inpatient setting. “Paradoxically, I think for mental health the mobile-type approach is more applicable in inpatient settings, because on a ward you’ve got lots of regular tasks,” says Reed. He contrasts this to community mental health provision, where work tends to involve very complex conversations which necessitate recording more than yes/no information.
Indeed, the trust has already sought to make use of mobile when it comes to therapeutic observations on wards. “We’ve done some in-house development and now have staff with various devices – phones or tablets – that give them a very carefully designed, process-driven interface for them to know who’s meant to be observed and when, and it presents information [about the patient] with a photo and their care plan, so staff know exactly who it is.
“That’s working well – we’ve got it on one ward at the moment, and it’s rolling out across the trust now.”
He also sees potential to do away with the traditional hardcopy ward diary – “which in most wards is still a book that sits in the office and lists everything from the man who’s coming to fix the radiators to if someone’s going to be out for the day” – and move to mobile.
“That concept of a digital logistic management system is something that would have a lot of value. At the moment, the clinical record systems obviously don’t really concern themselves with things like ward management logistics – it’s not really what they’re about; they’re about patient data. But it’s part of running a hospital.”
Resarch value
So too is research, audit and quality improvement. It’s another area which might not immediately be thought of in the context of mobile working, but where some are already seeing benefits from grabbing a phone rather than a pen.
Among them is Yassar Qureshi, a surgical registrar at University Hospital College London Hospitals NHS Foundation Trust. He and his colleagues were keen to ensure consistency of care for patients who had undergone oesophago-gastric surgery, with a view to reducing the risk of complications or avoidably long hospital stays. A paper booklet was initially created to record a patient’s progress and ensure best practice was being followed.
“But it was subject to the same problem as documenting in the notes,” reports Qureshi. “Pages went missing, entire booklets were lost, and when conducting research and audit, someone had to still go and collect all the data and compute it. Inevitably, this meant much of the work we were hoping to achieve wasn’t completed.”
Evolving definitions
So the team moved its work to a digital platform – namely, an app. “It was developed with several ‘pages’,” explains Qureshi. “Each page represents an interaction with the patient, and there are several milestones that should be achieved by the patient on a given day. We simply tick the box if the task or milestone is achieved. This allows us to assess compliance against the pathway, which has been created based on best-evidence practice.”
He says the app makes such data collection much simpler. “More importantly, the data is automatically uploaded onto a database, negating the need for someone to manually enter all the data once collected. This has greatly improved the accuracy of data, and also is much more efficient when performing audits and research.”
South Gloucestershire Clinical Commissioning Group is another organisation which has found increased efficiency through greater use of mobile – simply by introducing the sort of electronic diary management abilities most take for granted in their private lives.
Home and away
“We’re a small CCG – only 50 people – and quite proactive, hands on, and operational,” explains Thomas Manning, the CCG’s head of information and performance. “And what we were finding is that more and more people were spending less and less time in the office, and that their daily schedules were changing without notice – so you’d got people turning up at the wrong places, or not turning up at all, just because the diary management ability and facility wasn’t really there.”
He adds: “Personally, myself, my wife and my son, we’ve got shared calendars – we all know what each other is doing. And it just seemed logical – we’re having this problem at work, why can’t we do what I do at home in the workplace.”
Staff were also clear, however, that they didn’t want to have to carry around a work phone with their work calendar and a personal one with their personal calendar. And so the CCG worked up a bring your own device policy, using a mobile device management solution to ensure information remained secure while giving users access to their CCG e-mail addresses on their personal phone.
The policy, initially implemented in 2014, has since been superseded by the full introduction of NHSmail at the organisation – it can be securely accessed on personal devices. But Manning feels lessons remain: mainly that for mobile working to be viable, it needs to take into account how individuals typically operate.
Cultural considerations
Reed’s organisation is not taking the bring your own device route. “I find it difficult to see the argument,” he says. “It just seems like a lot of hard work, and you get into difficulties over boundaries between home and work, and security risk.” But he fully agrees that, for mobile working to be properly adopted, there are cultural considerations as well as technical ones.
He gives the example of his trust’s nursing staff moving from office-based to fully mobile. “They are in a pattern of work, and it often involves coming back to the office to write up their notes, and now we’re saying actually you don’t have to do that any more. But there are other reasons you want to come back to the office apart from typing up your notes.
“Managing that transition is quite difficult – to go from office-based to completely mobilised. I don’t think we’ve done that yet, and that will probably take a long time to happen across the board.”
Making mobile strategies a success

By Ian Bailey – District nurse, Queen’s Nurse and head of customer operations for EMIS Health
The right information, in the right place, at the right time. It’s something that all clinicians know the value of, but it’s become a particularly important adage for those in community healthcare settings. The changing landscape and agenda that’s driving more care out of hospitals has, for many years now, increasingly raised the requirement for community healthcare professionals to have access to clinical records wherever and whenever they’re providing care.
So why hasn’t there been a widespread adoption of mobile technology to make this information readily available? Certainly, costs play a large part. Devices, software, licences, connectivity and security all add up and create challenges for organisations. And then there are issues around lack of resources and technical barriers.
But from my experience, the challenges that are hardest to address are the cultural and human ones. Whether it’s sticking to old practices because ‘we’ve always done it like this,’ fear and unfamiliarity, or worry around ‘yet another change’ to manage, these are often the issues that remain unresolved and act as very real barriers to the use of mobile technology.
Unfamiliarity, tradition and fear
Domiciliary visits are steeped in tradition for numerous clinical disciplines. For many years, a visit from the GP, district nurse, midwife or health visitor has been a familiar part of many patients’ care. And in relatively more recent times, these methods of delivering care have become familiar for several other clinical disciplines too.
But Lloyd George notes (or more recently, a print-out of the patient summary) and patient-held nursing records are part of this tradition, and are still far more commonly used than mobile devices. Clinicians who were taught to use paper records are comfortable continuing to use them to support their interactions and working practices.
Tradition is rooted in comfort and comfort is rooted in fear. Which is why, when we consider the challenges of delivering face-to-face care, it’s understandable that healthcare professionals stick to what they know. They encounter emotive conversations, challenging situations and high expectations from both patients and carers, and for many, these challenges are amplified when technology is added into the scenario. Concerns over devices crashing, screens freezing, a lack of connectivity, or the fateful ‘password amnesia’ that occur at just the wrong time, all add to the fear of using mobile technology as a routine part of patient care.
Pushing past these concerns
The reality is, however, that once these fears and concerns about the unfamiliar are pushed past, mobile technology can actually help to improve patient interactions and lessen the challenges of face-to-face care.
I’ve spent many years in various healthcare settings, documenting the care that I’ve provided on various media types. My experience of using mobile devices during clinical interactions has demonstrated that it can create a level of enthusiasm and interaction from patients that cannot be derived in other ways. Showing a patient a graph of their recent blood pressure results, a copy of their recent hospital discharge letter or their X-ray image allows for another level of therapeutic interaction, involving the patient and firmly placing them at the centre of care.
So while clinicians often raise the concern that a mobile device would be a barrier to their interaction with patients and the therapeutic relationship they have with them, it’s my belief that these points are raised as a further consequence of fear and unfamiliarity.
Overcoming human and cultural challenges
What’s clear is that, in order for mobile devices to be widely used and for their benefits to be realised, there needs to be a change in mindset.
So what do we do to change attitudes and how do we help healthcare professionals overcome their fears? While their concerns are individual and personal, they feed into a wider culture that needs to be transformed. Ultimately, we need to immerse clinicians in a culture that allows them to change, gives them permission to voice their fears and lets them overcome their unfamiliarity.
In order to achieve this shift in culture, there needs to be people within organisations who share an enthusiasm and vision to drive changes. Which is why CCIOs – and other clinical champions of technology – are important.
The importance of clinical leadership
As a clinician, you’d expect me to preach the message that all clinical technology programmes absolutely have to have clinical involvement. But I think we also need to go further and ensure that all programmes are clinically led.
The emergence of the CCIO role has gone a long way in a relatively short space of time to address this at a strategic level. With the successful leaders that we now have within this space working to advance the role, professionalise it and take it beyond its traditional medical roots (the increasing emergence of CNIOs are a good example of this), we’re already realising the benefits of technology programmes for a wider population of clinicians and their patients.
It’s with robust strategic leadership that clinical informatics can permeate across all levels of an organisation. But there are also leaders at lower levels in organisations that can help to embed these cultural changes.
While the introduction of clinical informatics champions remains relatively small, they’re helping to improve the adoption of new technology. Working in hybrid roles and often achieved through part-time secondments, these positions are allowing clinicians to maintain their usual clinical role while being able to share knowledge of their service. It’s something that is providing not just ‘on the ground’ support for clinicians, but is also improving the development and configuration of technology.
Making mobile strategies a success
Changing long-ingrained beliefs might seem like a mammoth and daunting task, but these clinical leaders can be the key to the successful adoption, ownership and use of mobile technology.
They occupy a unique space within care organisations that allows them to bridge the gap between tradition and innovation, thanks to both their personal insight into the challenges that clinicians face and their understanding of the benefits of mobile technology.
With these champions working alongside clinicians and listening to their concerns, they can start to dismantle the personal fears that surround using technology at the point of care. By chipping away at these barriers, clinical leaders can move care beyond tradition and transform the wider culture, so that technology is more widely adopted – to the benefit of both clinicians and their patients.

|
|
| Contact number: +44 (0)79 1765 8225 Email: ian.bailey@emishealth.com Our website: www.emishealth.com Twitter: @emishealth LinkedIn: www.linkedin.com/company/emishealth/ Facebook: www.facebook.com/emishealth Further reading: Saving an hour a day with EMIS Mobile Beyond apps – how to delivery mobile healthcare [ssba]
|
|
Making mobile work – securely

By Gregg Hardie – Head of Public Sector, Samsung
At Samsung, we are keen for those working in healthcare to be able to reap the benefits of mobile working. We believe it can and will make a real difference to their level of efficiency and the satisfaction they take in their job.
We also know, however, that its introduction is not without challenges. While there are already numerous examples of care being improved through the use of mobile technology – whether community nurses are able to better manage their administrative workload, doctors able to remotely view observations data and speedily spot and respond to deterioration, or even patients able to more easily share information with their clinicians – there can also be risks to mitigate? Chief among them is security.
It’s a concern which is perhaps particularly pressing for information technology departments. The growth of clinical uses for smartphones and tablets means more devices to manage within an organisation. And the desire from staff to use at work the technology they take for granted at home means those devices aren’t’t always just the ones carefully selected and procured by the department. Meanwhile, the WannaCry global cyber-attack has put cybersecurity in the NHS – or the failings thereof – on the front pages of national newspapers.
At Samsung, we want to ensure that mobile technology is used to improve healthcare. But we also want to ensure staffs are able to use such technologies in a way which keeps patient data safe. We know our colleagues in healthcare IT departments want both those things too.
That’s why Samsung’s security platform, Knox, is built into every mobile device we provide. It’s also why we offer additional Knox solutions which make it quick and easy to tailor devices for use in healthcare settings.
It is vital to have ensured the confidence risks of data breaches are mitigated. But creating devices which are so secure as to be impenetrable to users is not an option. Data needs to be easily accessible at the point of care to the people who need to see it, and easily updatable. Security cannot become a byword for unusable. If it does, one of the major benefits of mobile working – increased efficiency – is negated.
The issue of keeping patient data safe is of course not a new one. But it’s becoming more complicated as information is stored on devices which move around with the people using them. There is also the issue of needing to share information with a wider number of users over a wider geography.
To address the challenges, healthcare organisations will need devices which have sophisticated security settings which can be easily tailored to the healthcare environment. The ability to perform over air updates will be essential, so as to be able to speedily apply security patches and relevant settings for specific staff groups without the need to directly access the device. Organisations might also consider devices which offer the ability for ‘dual persona’ setups, through which personal and work applications on a smartphone or tablet are separated: a valuable way in which to make bring your own device a more manageable prospect.
Mobile suits the way healthcare operates now, but it will only be viable if we get security right. Healthcare professionals and patients will expect nothing less.

|
|
| Point of contact: Helen Shaw Contact number: 078 9687 3125 Email: h.shaw@samsung.com Our website: www.samsung.com [ssba]
|
|
Mobilising health and care

By Servelec
With efficiency and modernisation at the forefront of the health and care agenda, mobile working plays a key part in achieving these efficiencies, helping clinicians to provide a higher standard of care and at the same time delivering the ‘paperless by 2020’ agenda.
NHS Trusts and local authorities across the country are faced with budgetary constraints and are under pressure to meet higher demands with limited resources. Servelec HSC believes that with the appropriate mobile tools in place our customers can work more efficiently and effectively, wherever they are.
In health and social care, considerable resources are invested in case management, administrative or clinical systems and we are prioritising how we can maximise benefits and focus future investments on areas that will deliver the greatest impact.
We are in no doubt that modern mobile technology is the future of effective care delivery. With this in mind we are working with our customers across health and social care to develop mobile solutions that deliver results. We have engaged with specialist applications developers to ensure that our suite of apps are modern, user friendly and relevant to the role of the user.
Achieve greater efficiencies and outcomes
Health and care services are rapidly recognising the need to work in more efficient ways to increase productivity, and the opportunities offered by mobile working are boundless. Our modern Rio mobile platform enables frontline staff to make better use of mobile technology, this means health and care services can:
- enjoy the convenience of having the relevant information, they need for their role and their patients, at their fingertips
- deliver more value, adapt and respond more quickly with access to real time information
- improve health/outcomes, transform the quality of care and reduce the cost of services
Smart APPlications; information at your fingertips
To help drive improvements and efficiencies, it is essential to adopt a forward thinking approach and use the right tools to deliver the right information to the right person at the right time. This will help to improve the individual’s outcome and their experience with the care provider.
Frontline staff in health and social care services are constantly on the move and rarely sit down in front of a desk with a computer. Our Rio mobile platform offers a modern solution that delivers a more personalised and efficient experience, as the user has access to task lists that are relevant to their role – whether this be for a community or district nurse, health visitor or social worker.
Working with our specialist mobile app partner on the creation of our first role based apps, the user friendly application will enable frontline staff to work effortlessly whilst on the move. Tailored to the user’s role / specialism, features on the app enable frontline staff to manage appointments, view patient information, record clinical notes and assessments, maximise visits/mileage using the integrated map on the smartphone, and manage patient alerts.
Servelec is the only company in the UK to work with Global Digital Exemplar (GDE) Trusts in both the secondary care and acute care settings. Our customers who are awarded GDE status are recognised for their digital maturity and excellence and will act as exemplars for how the rest of the health service can make better use of technology. They will also provide a blueprint for other Trusts going forwards to help to improve the quality of care and the patient experience.
To find out how our modern mobile solutions can help mobilise your workforce, please contact a member of our team today.

Email: servelechsc@servelec-group.com
Our website: www.servelechsc.com
Twitter: @servelecHSC
LinkedIn: www.linkedin.com/company/servelechsc/
Further reading:
RiO: A feature rich electronic patient record (EPR) system created in close collaboration with clinicians.
Mosaic: Adults, Children’s and financial case management on a single platform.
Using the foundation of an Integrated Digital Care Record to improve patient participation and satisfaction

By Felim McCarthy – Senior Clinical Consultant, Orion Health
Orion Health’s Integrated Digital Care Record (IDCR) solution provides a single patient-centric view of health and care information, however access to it is often confined to clinical staff within an organisation. Even a view-only integrated digital care record can provide profound benefits in terms of improved patient care, reduction in a range of delays across the patient journey and improvements in overall efficiencies; however often the patient is neither aware of the record nor actively tasked to engage with it.
Health and social care is undergoing a transformation from intervention to prevention. Success depends on patients and their carer(s) playing a greater role. The more information patients can access about their care and the range of interventions they could take, the more likely they are to actually take those interventions. That is why Orion Health’s IDCR can be extended to a patient portal, accessible via the web or an app. Data collected from the patient portal is then fed back into the IDCR where appropriate, feeding the single view of patient information. The Orion Health platform has HL7®FHIR®capabilites for interoperability, so that the patient engagement solution can connect with other systems and apps.
Orion Health’s patient engagement solutions enable the sharing of data beyond organisational boundaries. Patients can actively participate in their care by managing appointments, tracking goals, completing online questionnaires and contributing data from wearables such as FitBit and Apple Health or other clinically relevant apps. Benefits can be seen across a range of use cases. For example, a patient completes a post-operative assessment via the patient portal removing the need to physically attend the hospital. For those in remote areas or travelling a long way for specialist treatment, this is a real advantage.
The ability to deliver and gather such data via a web browser or app whilst maintaining confidentiality and patient privacy opens the way for direct patient interaction with clinical and social care staff. In turn this supports grater engagement and can improve adherence in terms of treatment profiles, life-changing exercises and medication management.
Another key feature of Orion Health’s patient engagement solutions is Circle of Care, where a patient can connect with those involved in their care and treatment, including nominated family or friends. Patients can upload and share images and reports via the patient portal for their care team to access, and vice versa providers can share files and information with patients.
So is this wishful thinking or a reality? In the UK, Golden Jubilee National Hospital recently went live with a pilot, initially involving 40 pulmonary hypertensive patients who often travel a long way to attend the Scottish Adult Congenital Cardiac Service (SACCS). The Patient Portal provides these patients with a summary of their most up to date clinical records and related hospital appointments and allows them to share this information with other clinicians, for instance in their local area. Later this year, patients will be able to upload their own information and complete documents, such as follow-up questionnaires.
To find out more about Orion Health’s solutions for patient engagement, click here.

|
|
| Contact number: 087 0486 8406 Email: emea-marketing@orionhealth.com Our website: www.orionhealth.com/uk/ Twitter: @OrionHealthEMEA LinkedIn: www.linkedin.com/company/orion-health/ Facebook: www.facebook.com/orionhealth/ [ssba]
|
|
Illness doesn’t recognise boundaries – neither should healthcare

By Paul Jackson – Head of marketing, Agfa Healthcare
How should NHS organisations adapt to modern and mobile working?
Agfa HealthCare helps healthcare organisations deliver better care. We do this through a range of digital health products and solutions, and through our 100+ years of healthcare experience. Today’s digital health is the convergence of technologies, knowledge and skills supporting the transformation of health, social and informal care; without boundaries.
Digital health is a multidisciplinary domain which involves many stakeholders. Agfa’s Digital Health range covers four main product areas:
- Enterprise Imaging – VNA, Viewer, PACS, Image Exchange, Cloud
- Hospital IT – EPR/HIS/CIS, ECM
- Integrated Care – HER, care information exchange, image sharing, patient engagement
- Digital Radiography – medical devices such as direct radiography, computed radiography and image processing
As a supplier to the NHS for over 40 years, working practices and access to systems have changed dramatically over time especially the last decade as hospitals become increasingly paper-lite. Mobile access and working functionality are now expected and fundamental requirements of Agfa HealthCare’s Digital Health portfolio, an interoperable ecosystem of data capture, exchange, share and collaboration with advanced tools for analytics – the foundation for the transformation of health and social care.
Enterprise imaging
Taking our enterprise imaging solution, a single, sophisticated, unified imaging platform. Having all imaging data available from one single imaging interface across web and mobile platforms allows users to work where they want, how they want, letting clinicians view images, videos, studies and work on reports – even over low internet bandwidth. The ‘lightweight’ client lets users create, edit and approve reports remotely, from a mobile device. With real-time collaboration, the ways of direct messaging and sharing that we have become so used to using every day are available securely within enterprise imaging, enabling acquisition, sharing, reviewing and reporting on all kinds of imaging data. So whether it is collaboration inside or outside the hospital, chat and visual collaboration tools let a clinician and a colleague look at the same image, making mark-ups and measurements that both can see, all while communicating directly online.
Universal Image Viewer
Agfa’s universal viewer, XERO, provides secure access to imaging data from different departments and multiple sources, in one view, to anyone who needs it. The XERO footprint web viewer – which can be accessed on any Android or Apple device – allows clinicians to work on the go, capturing and uploading images.
The XERO footprint viewer also has received FDA 510(k) clearance for diagnostic viewing. This full fidelity view functionality of the viewer uses lossless compression to provide diagnostic quality when images are displayed, by retrieving original-quality renditions of stored DX, CT, MRI, CR and US images.
Using streaming technologies, information is displayed in the XERO footprint web viewer from the server, meaning that no patient information is stored locally on mobile devices.
Home working
Multiple options exist for home working and reporting with Agfa’s Enterprise Imaging platform. When connected to a hospital’s IT network through VPN, the user can report at home with the same toolset as in the hospital, using the full-features diagnostic desktop. Alternatively, the mobile reporting tool allows the user to report and sign-off studies within a web browser, also supported on mobile devices.
Electronic Patient Record
ORBIS, Agfa’s electronic patient record (EPR) solution provides functionalities as part of the ORBIS Mobile Edition (ME) on devices at the patient’s bedside and beyond, providing the clinician with relevant information, right where it’s needed. Using ORBIS ME clinicians can capture, share and access patient information from anywhere in the hospital on a tablet device. It provides a fast overview of the patient record and supports care providers during their daily activity.
The ORBIS solution has been carefully designed to provide the information that is really needed and offers an interface specially adapted for ease of use. With ORBIS ME, users can order radiology exams or new lab tests and at the same time consult results of earlier tests and view images/reports through an integrated web viewer. Prescription of medication is fast, secure and easy. Touch screen calendars make it easy to enter the date and time of drug administration. ORBIS ME provides access to information and alerts directly at the patent bedside, helping reduce the risk of errors and improving the workflow. Checking or capturing patients’ vital signs at the bedside is also easy with minimum typing and pre-set buttons. The ORBIS ME solution simplifies the daily routine activities of the caregivers, so caregivers can focus on providing better and safer patient care.
The era of integrated care
The healthcare industry continues to experience change at an unprecedented rate. Change is not only occurring in the technology used in diagnostics but also in care delivery as organisations move towards fully integrated care involving all members of the healthcare ecosystem – patients, providers, clinicians and caregivers.
Agfa’s Integrated Care Suite is an enabler for connected care and the convergence of information and technologies, improving patient and population outcomes and the patient experience.
Illness does not recognise borders and boundaries, neither should healthcare. Today’s hospital networks may cover multiple sites but different care providers need access to all of a patient’s data, from any facility, hospital, department, region, wheherimages, lab results or clinical notes.
The Agfa Integrated Care Suite can provide access to all the patient data in a single overview and enable treatment to be given closer to home, enhancing patient comfort and care, with technology enabling a seamless transparent and real-time communication of healthcare information such as reports, data and images. This information can be easily accessed on mobile devices via commonly used browsers. In addition, when results reveal a critical or urgent situation, clinicians immediately receive an alert on the mobile phone app. They can access and read the entire report, no matter where they are, on- or off-site. For more information visit the Galway Xperience.
Patient engagement
Patients today need and want to be more involved with their care. When patients are more in control of their own healthcare, they become engaged. For example, that they are more likely to correctly follow their treatment and take care of themselves. Greater involvement by the patient can translate into better outcomes, and a patient portal has a key part to play in enhancing this involvement.
Patients and their health teams need to be able to communicate with each other conveniently and quickly, while patients also want to be able to access and share their own data. And they expect the same mobile functionality they now use in all parts of their lives.
The hospital itself can benefit from this information exchange: by making it easier for patients to find information and even fill in forms and questionnaires before arriving at the facility, the reception and patient flow are faster and smoother.
Agfa HealthCare’s flexible digital health solutions provide healthcare organisations with modern, mobile and secure ways that help deliver better care.
For information on Agfa HealthCare, contact Paul Jackson via:

|
|
| Contact number: 084 5680 3249 Email: paul.jackson@agfa.com Our website: www.agfahealthcare.com Further reading: Galway Xperience [ssba]
|
|
Acute Mobility – Think big but start small…
By CGI
The Problem
Hospitals have a wealth of patient information such as lab and imaging results and patient documents held electronically – but all too often these are held in separate disconnected systems and accessed via aging desktops which can be difficult and time consuming to use.
The Solution
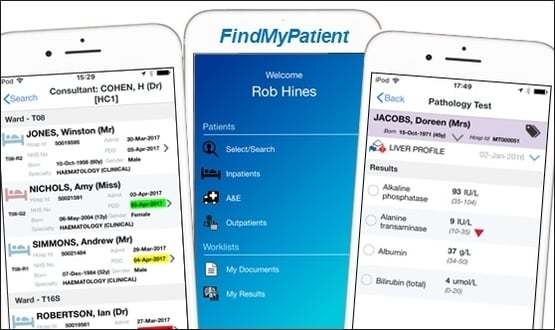
CGI’s mobile app, FindMyPatient not only brings this information together, but presents it in an intuitive way to the user’s mobile device. This approach unlocks the critical information held in a trust’s existing ‘best of breed’ systems and allows users to easily access a real-time consolidated view of the patient data on a handheld device.
The app was originally designed in response to a simple problem from a Clinician “when I’m on the move, how do I find my patients when they are scattered across the hospital?” – and has evolved to include:
- Patient activity: Inpatients, Outpatients and A&E
- Clinical Information: Pathology and Imaging results, Documents/Correspondence, Alerts & Allergies.
- Workflow: Results inbox, including acknowledgement and tagging
- Managing Patient groups: at individual user level and as part of a clinical team
Benefits
The benefits demonstrated by our clients are:
- Saving time: 30mins per user / day through information available at the point of care, and not having to find then gain access to the information on a desktop PC – allowing users to have access to key information ‘on demand’, at the right place.
- Better Decision Support: Information can be accessed real-time to support clinical workflows e.g. by checking the latest patient results during a ward round. On average users access information 3 times more frequently compared to the desktop application, and 5 times more frequently out of hours.
- Safety / Compliance: Access to clinical information when away from the hospital to support out of hours care and, providing easy facilities to mark Results as ‘read’. 100% of users stated that it improved patient safety.
- Staff Experience: Convenient access to information enables staff to focus on the job of caring for patients and removes frustrations of existing IT solutions.
- Patient Experience: Improved patient confidence in the service and engagement in treatments via sharing information on the app at the bedside.
Feedback
Richard Cohen, Colorectal Consultant at UCLH, commented on the difference the app has made to his work:
“I’ve been using FindMyPatient for the last few months and have found that it has made a real difference to my ability to access information on my patients. The app is a great example of how well-conceived IT can help clinicians balance the pressures of modern healthcare. One of the great advantages is that I can use the app outside the hospital to review the patients under my care, which was previously complicated. The app is a real step forward in facilitating patient care.”
Other feedback from clinical users:
“This is going to transform my ability to care for patients”
“This app is brilliant. Easy to use and info is great.“
“It is sensational.”
“This app is a life-saver. I work across multiple sites in other trusts and I wish they all had something like this.”

|
|
| Contact Number: 077 9695 6371 Email: Owain.donovan@cgi.com Our website: www.cgi-group.co.uk Twitter: @CGI_UKNEWS LinkedIn: www.linkedin.com/company/cgi/ Facebook: www.facebook.com/CGI.UK Further reading: Hospital app tracks patients [ssba]
|
|





