Think tank calls for prescribing rights to be extended to Singapore’s GPs
- 5 March 2024

A think tank has suggested that Britain should extend prescribing rights to Singapore GPs and look to Singaporean polyclinics in efforts to boost the ailing NHS.
Britain’s troubled NHS makes headlines regularly. But could salvation come in the form of Singaporean-style polyclinics and allowing Singapore GPs to prescribe to Brits? Social Market Foundation Think Tank believes so, setting out its vision for the future of the NHS in its recent briefing paper, What the NHS can and cannot learn from the Singaporean health care system.
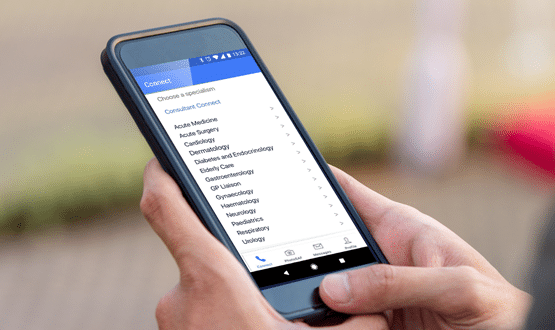
The paper suggests that permitting online doctors from Singapore to consult with British patients and prescribe medicines to them could reduce the pressure UK GPs are under. In a country where accessing GP appointments is increasingly difficult, a move like this would also open up access to patients in areas where access to medical care is poor.
In addition, the paper praises Singapore’s polyclinics as being a key part of the renowned efficiency of the country’s healthcare system. It suggests they should be introduced to the UK as a cost-efficient solution to tackling backlogs and lengthy waiting lists.
Former health minister Lord Norman Warner penned the foreword to the paper, writing that it provides: “valuable service delivery ideas that would help rescue our beleaguered NHS. It also contains some interesting ideas on how citizens can build up funds through an insurance system to make out of pocket payments later and reduce the burden on taxpayers.”
Singapore leads the way
According to the paper’s author, healthcare researcher Max Thilo, Singapore spends 4.4% of its national income on healthcare. By comparison, the UK spends more than twice that. Yet, despite this, it is the small city-state of Singapore that has an infant mortality rate that is half of the UK’s; has far lower levels of obesity than the UK; and a life expectancy of 83, compared to the UK’s 81.
The healthcare system in Singapore charges patients to access services, which the author believes goes some way to moderate demand. Additionally, it takes a population health approach to the delivery of health services, and crucially services are not centred around acute hospitals.
Singapore has poured investment into polyclinics and telemedicine. As a result Singaporeans tend to visit their GP more often than English patients. And when they do it is outside of acute hospitals – which by their nature are the most expensive part of a healthcare system due to fixed overheads and expensive maintenance.
Polyclinics to ease pressure
Polyclinics combine GP services with other healthcare offerings, such as diagnostics or healthcare teams managing chronic conditions. The idea has been explored in the UK before under Gordon Brown’s government, though it was quickly shelved in the early stages. Now the paper is calling for it to be considered again.
Thilo writes: “There is significant variation in access to GP services, both between and within integrated care boards. Singaporean polyclinics offer lower unit costs and pay their doctors more than English GP practices. NHS England should therefore trial Singaporean-style polyclinics in areas with poor access to primary care services, and allow doctors to share in productivity improvements through higher pay.”
By separating acute and chronic patients, polyclinics can operate at higher volumes, seeing more patients. In Singapore, polyclinics provide subsidised primary care services to 20% of citizens, focusing on low-income patients with chronic health conditions. More recently polyclinics have adopted a ‘teamlet’ model – with each patient signing up to a teamlet consisting of two doctors, a nurse and a health coordinator. This style of consulting is also helping doctors to see multiple patients at one, as each member of the teamlet can see a patient simultaneously.
Opening up prescribing rights
The paper also calls for the UK government to consider liberalising prescribing rights for Singaporean telemedicine providers. With more and more British patients struggling to get an appointment with their own GP, many are turning to private care and telemedicine options. In the UK private appointments can range from £50-150 putting them out of reach for many. Similarly, online appointments can range upwards from £29. By contrast, Singapore’s leading telemedicine provider, Doctor Anywhere, offers its services from £12.
Thilo argues that by granting UK prescribing rights to Singaporean doctors, affordable telemedicine and a high standard of healthcare can be accessed by low-income patients in Britain.
Such a change would likely require the UK to grant Singapore a data-sharing adequacy decision – however, Thilo points out that Guernsey has recently been granted one.



1 Comments
Don’t you just love the headline? Has anyone stopped and thought that perhaps GP practices here are actually working at amazing levels of efficiency already for 17% less in real terms than 5 yrs ago. All the published evidence shows this. Sure we can all do better, but how about funding the sector properly? Declaration of interest-I am a front line GP working in a top 50 patient satisfaction GP practice (IPSOS 2023) and am fed up with dumping from the rest of the NHS on me-up to 20% of my daily grind is doing work that others should be doing, yet they all blame me. Best one yesterday was the local gynae department that last week saw a frail elderly patient, undertook a procedure and immediately discharged her saying “any problems go and see your GP”-and there were and she did.
Comments are closed.