Health IT and Vitality
For somebody used to the hubbub of a practice in south London, the Vitality Partnership clinic at Enki Medical Practice in Birmingham is eerily quiet on a Friday morning.
A couple of people wait on the comfy looking chairs in reception, while someone else uses the touchscreen monitor to access general health information; in this case, advice on smoking cessation. The only other people in the room are the receptionist staff.
It was a very different story two years ago, explains Jayne Hunt, head of operations at Vitality Partnership, who says that some practices in the region would have queues of more than one hundred people in the morning.
The lines would stretch all the way out into the street, and doctors would be rushed off their feet trying to deal with the constant stream of patients.
Since then, Vitality, a GP super-practice covering 13 locations in Sandwell and Birmingham, has revolutionised the way it works.
It has created a single clinical contact centre for its practices, offering online appointment booking and registration, providing locally-focused information online, and allowing patients to opt for consultations by phone or Skype.
Rising to the Challenge Fund
It’s an impressive transformation and one that has only been made possible through innovative use of technology, integration of services, and investment from the Prime Minister’s Challenge Fund set up in 2013 to support innovative ways of working in primary care.
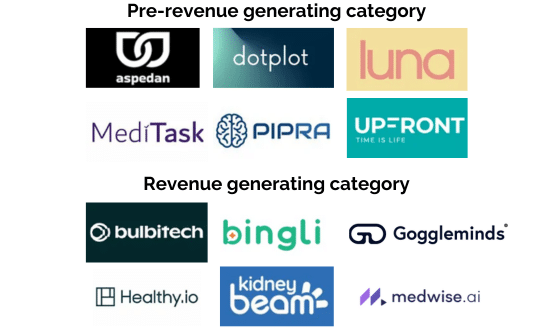
The recipient of the fund was Health United Birmingham; a collaboration between Vitality and Digital Life Sciences, a local tech company with a focus on healthcare.
Hunt explains that Vitality and DLS had been partners for some time and the transformation journey started long before the Challenge Fund was announced, but: “When the Challenge Fund was announced it felt like an ideal opportunity.
“Here is a vehicle that we can use to put into practice some of our thoughts. We knew what we wanted the tech to do, and we needed DLS to work with us do that.”
A new way of working
At the heart of Vitality’s new way of working is a new clinical contact centre to handle appointments. Previously, patients who wanted to book an appointment could ring their local practice, which often had long waiting times, or physically turn up on the day, leading to those huge queues.
Now, when patients ring their local practice number they are now given a choice as to whether they want to see a GP or want a more general service, such as a prescription renewal.
If they choose the latter, they are transferred to someone at their local practice, but if they want an appointment their call is handled by one of the staff in the centre – most of whom have experience in 111, 999 or another busy call centre.
After speaking to them, patients are given the option of booking either a face-to-face consultation or a remote consultation via phone or Skype.
It’s a process that is working exceptionally well, says Hunt. “Within a month of going live we had four people in line [outside practices in the morning].
“That was a massive reduction in pressure for reception staff and clinicians.” Now, around 65% of all health concerns are dealt with remotely.
Expanding access
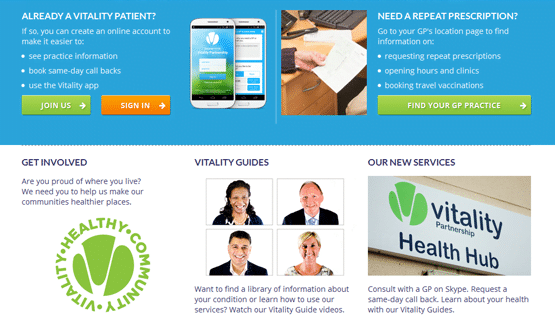
As might be expected in any other industry outside healthcare, patients also have a genuine, workable and effective way to access Vitality’s services online. This includes the ability to book appointments on the revamped Vitality website or on a free app.
Vitality now gets on average around 50 appointment requests through its online channels a day, around 25% of which come via the app.
Other online support includes a series of video guides covering key areas, such as living a healthy lifestyle, skin conditions, throat problems, and life as a student (Birmingham City University is covered by two Vitality clinics).
For all of these videos, the team uses local GPs that patients will recognise, believing that this helps to build trust in the service.
“This isn’t something from NHS Choices. There are people familiar to patients,” says Hannah Mae Lewis, business development executive at DLS.
These videos can be another resource that call handlers can recommend to patients; and Hunt says the partnership had considerable success with a video on flu vaccination last winter.
For people with long-term conditions, such as diabetes, clinicians can also prescribe specific suites of online videos that are sent via email.
In this whole process, DLS and Vitality considered the multicultural nature of Birmingham’s population, and videos are available in Punjabi, while the main website is available in four different languages.
Another option
The reason for all these tools is to give patients more options, rather than move them keep people away from their GP, says Lewis.
“It’s all about access and allowing people to see their GP when they need it. Pointing in right direction and getting to the most appropriate place.”
Ryan Smith, central operations manager at Vitality, agrees: “What we’ve done is offer more access options rather than remove the traditional option and put this in place.”
Not everything has the impact Hunt and her team might have liked. Despite the enthusiasm of policy makers and ministers for Skype, they have found that demand for video consultations using the online service is relatively low; perhaps because it is easier and more convenient to just make a telephone call.
Skype does come in handy in some specific instances, says Lewis. For example, if English is not someone’s first language, they can ask a family member or friend to join the consultation.
The team would also like to do a lot more on the social media front, with current usage limited due in part to lack of marketing budget for the project.
The differences
On the whole though, the statistics are impressive and a sign of real change for primary care in Birmingham.
To track changes DLS has created a dashboard to track various usage statistics, the top line results of which are sent to Mott MacDonald – the consultancy firm that NHS England commissioned to assess progress of Challenge Fund recipients.
There are now 700 calls per day taking by the clinical contact centre, with calls answered on average within 40 seconds. This compares to the previous average wait time of six and half minutes.
The actual time a patient spends on the phone has also been significantly cut from ten minutes to two minutes, as needs are addressed more quickly.
As for the actual consultations, the average phone consultation is five minutes, compared to a traditional seven minute face-to-face consultation, allowing GPs to see more patients per day.
An unexpected benefit has been the drop in missed appointments, with DNA rates falling by 70% – a change that Hunt puts down to the reduction in time between setting up a consultation and the consultation taking place.
Perhaps most significantly of all, rather than seeing fewer patients, the new way of work has allowed Vitality’s practices to increase its capacity by 10%; a figure that may have been on Prime Minister David Cameron’s mind when he used the Vitality practice to launch the Conservative’s plans for a seven-day NHS.
Smith says: “We’ve felt an increase in handling without putting more into system; just by making appointments more efficient. We’ve created 10% more capacity in core hours rather than extended hours.”
Now in the vanguard
In addition to being a Challenge Fund site, Vitality has also been announced as one of the 29 ‘vanguard’ sites that will test out the new models of care trailed in the ‘Five Year Forward View’ plan to try and stave off a £30 billion funding crunch by 2020-21.
Specifically, it is a ‘multispecialty community provider’ vanguard, with a goal of expanding the range of social, mental, community and enhanced secondary care services on offer to patients by delivering community outpatient and diagnostic services.
“It’s about how do we work together to provide a more coordinated approach,” says Hunt. “So as far as patients are concerned it doesn’t matter which door they go into, we are all working together and the best person that needs to work with that patient is the one that works with them.”
Hunt says the Challenge Fund work has been a “very good grounding” for their status as a vanguard, with data sharing agreements between practices already in place.
The work now includes making sure the technology all those different areas talk to each other by working on interoperability.
“The reality is that nobody going to come up and put everyone on single system. We do live in the real world where mental health trusts use a different system to community nursing service and primary care.”
However difficult, it’s a task that Vitality is taking forward with gusto. “I don’t think there are as many other primary care organisations that are as forward thinking and ready to accept digital transformation as Vitality,” says Lewis. “[It has] real vision.”