Doctor’s union chairman calls for GP at Hand to be “scrapped immediately”

The chairman of a doctor’s union is calling for GP at Hand to be “scrapped immediately”.
The free NHS service, powered by Babylon, allows patients to book appointments and talk to their doctor through their smartphone within minutes.
It also claims patients can get a same or next day face-to-face appointment if needed at five clinics around London.
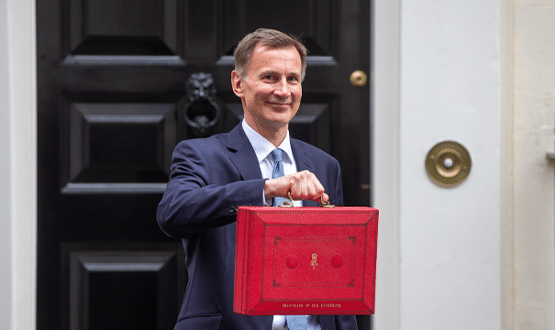
In a letter to Jeremy Hunt, signed by more than 130 health professionals, Doctors in Unite (DiU) – which is part of the Unite union – said signs up for GP at Hand have caused list sizes at GP practices to fall for the first time “in years”. When patients sign up for the service, they automatically de-register from their old practice.
The letter reads: “There is no doubt that GP at Hand will destabilise other practices, robbing them of the vital risk pooling and cross subsidy which enables them to provide good care to their more complex and unwell patients.”
The letter also accuses GP at Hand of threatening the model of general practices by “hoovering up” younger patients.
Chairman of DiU, Dr David Wrigley, said: “An increasing number of GPs are in open revolt at this online service that is seriously eroding the vital personal relationship between GP and patient, as envisaged when the NHS was set up in 1948.
“The model of care used by GP at Hand should be scrapped immediately.”
When contacted for comment, GP at Hand defended their service.
A spokesman said: “People have the right to choose their NHS practice. GP at Hand is an NHS service; paid for by the NHS; providing NHS services to all patients – just like the vast majority of GP practices throughout the UK.
“In seven months, over 40,000 people living or working in central London have applied to join NHS GP at Hand, with more than four out of five people rating our digital appointments giving them the full five stars. The average waiting time for an NHS GP appointment with GP at Hand is 38 minutes, compared to waits for routine appointments in traditional practices of a week or more.
“The reality is that patients and GPs are flocking to GP at Hand because they recognise the potential that high quality, digital-first 24/7 NHS GP services bring. The 200 GPs who have already joined Babylon do so because they are treated with respect and not put under the levels of pressure all too common in other practices.
“GP at Hand receives the same funding from the NHS as the vast majority of NHS practices do. The cross-subsidy allegation shows a failure to understand the basics of how NHS practices are funded.”
This is not the first time GP at Hand has been met with criticism.
In March 2018, Digital Health News reported on how a group gathered in east London to protest against the service.
GP at Hand was accused of draining resources from NHS practices with protesters holding up banners reading ‘GP at Hand should be banned’ and ‘GP at Hand not in my land’ while there were also similar chants against privatisation of the NHS. (A picture from the protest can be seen above.)




23 Comments
GPs providing their own apps ? That would be a disaster: 1. The level of service offered by different GPs is already very varied, encouraging them to do their own thing would make it even worse 2. GPs are far to busy to be doing this, best to stick to what they have been trained to do 3. We have a NATIONAL Health Service and technology and DATA should be being used to provide a level playing field (GP @ Hand or equivalents, should be available throughout the whole country).
Isn’t this exactly the sort of thing that disruptive technology is supposed to do?
As much as anything, the advent of GPAH highlights how far the current funding system is from being fit for purpose.
GPs shouldn’t have to be cross-subsidising anyone, surely that isn’t their role? Ideally they would be paid for clinical outcomes – but that might undermine GPAH’s business model.
As a GP I’d happily work for GP at hand. GP ran by the NHS is a disaster. Working conditions sound much better with GPAH and patients seem to like it.
The GPs complaining are the ones at risk of losing income / paying redundancy for their staff, so of course they won’t like their patients and money going to another service. The solution isn’t to kill GPAH, but to change the funding model.
……or for those GPs to embrace change and look to their GP system vendors provide the same app service… potentially negating the need for patients to flip over to GP at Hand.
Disagree. Read the Wachter report. GPs have always been the people at the fore front of using IT in the UK. Our systems are way more advanced than the hospitals who are still lugging around paper notes.
In any case. What are GPs meant to do? They have no say over what IT is procured on their behalf. In my CCG all the IT is bought centrally by NHS England. There’s not much a bunch of GPs can do to change what services are available to patients.
This is why it’s a good thing that there are people like GPAH around. Stuff like this forces change and possibly new technology to be adopted rapidly in different areas.
Disagree??? Can’t see why. If my GP offered the same online equivalent of GP at Hand as an option we would be delighted. They do offer telephone appointments if you can get one during the mad scramble for that day’s appointments between 8:00am and 8:10am each day. A minor step into the virtual world…. One small Tring Tring for mam, one giant leap for GP at Hand. Groan….
Yes, disagree. To hone in on a few points:
1) GPs aren’t opposed to change. They’re usually the first to try anything. The Wachter report backs this up and also the fact that GPAH allows you to see a GP, meaning there must be many GPs such as myself that don’t mind new tech at all.
2) GPs use the tech that’s available to them. In my CCG the tech has been procured by NHS England. In the area that GPAH is currently running the CCG must have procured GPAH for their area.
My point is that GPs can’t just set up a new service without any help from the powers that be. What do you expect from them? To do unpaid work in setting up new services so that they can hang on to their already dwindling take home pay? Get real.
Given the obvious popularity banning GPAH is must be the wrong response. But it does need a creative response from NHS England and DHSC to counter the risk of destabilising the entire primary care funding and commissioning model.
Ah… I see difference here re “unpaid work”. I was looking at this from the perspective of a NHS hospital employee who does not get paid extra on top of their salary to introduce innovative new EHR systems or loose salary by doing so. Just have do the day job and that too. No overtime paid either. Of course the govt/hospital provides the funds to pay the hospital EHR suppliers, employ the teams, etc (as could occur here too, obviously). Am I right that your perspective is that unsalaried GPs are different though and need to be financially compensated for time invested on change projects which would be at the expense of time spent earning money from patient care activity? Also is the payment for a face to face appointment the same as a virtual one? Not my area ….so explanation of “dwindling take home pay” would be good.
My view is that GPs carry out the duties in their contract provided by the CCG /NHS. There is no financial incentive for GPs to create a new service and take on all the risk along with it.
If the CCG push for it and provide funding then GPs will do whatever they’re asked to.
The fallacy here is that people think that a) GPs are trying to avoid new methods of working and b) if GPs don’t keep up then they’ll be the ones to suffer / go out of business.
In reality most GPs a) couldn’t care less because they’re not going to do work which doesn’t pay and b) no matter what the method of seeing a GP will be, GPs will be fine because there aren’t enough of them and no matter what they decide to do, they’ll find a role while pays very well. It will be the patients that suffer when practices continue to close.
In terms of how GPs get paid. The GPs who are partners get a fixed amount of money per patient per year. They don’t get paid per patient contact. It’s a set amount and they have to do as much work as needed to get through the day – there’s no limit to the work. Video consultations as I understand are remunerated by patient contact / the hours worked. So GPs will make more money by working for services like GPAH.
Inflation has increased, staff costs have increased to run practices, indemnity has increased, work load has increased. This has resulted in GP partners taking home 10% less in real terms than they did ten years ago.
Great idea – let’s hope GP at Hand makes its way up north ASAP. Have severely disabled daughter with complex and serious health needs – If my wife doesn’t manage to get through to our GP receptionist within 5-10 mins starting at 8am all the appointments are gone. So frustrating.
GPAH are providing a service that people want or they wouldn’t have the large numbers of people that are currently signed up. On that basis alone, there is no point in trying to shut them down – the people have spoken. The genie is already out of the bottle. Yes there are clearly issues around cherry picking the younger ‘easier’ patients and the funding model but GP’s should focus their energy into raising their own game rather than trying to bring their opponents down.
GPAH have weaknesses in that they are not able to deliver a fully inclusive service as has been highlighted in earlier posts. e.g. currently if a woman joins GPAH and becomes pregnant, she will then have all the issues of having to register with another GP. What a hassle! I can imagine that that issue alone would affect a sizeable amount of GPAH’s so called ‘younger patient’. So what’s so difficult then for GP surgeries to start providing a similar service, but market is as being a more inclusive, more flexible, in a word ‘BETTER’ ? e.g. if a women became pregnant she could still stay with the SAME SURGERY during that period and then go back to video consultations later on at the SAME SURGERY.
GP’s can not only ‘join them,’ they can ‘beat them’ if they have the energy and drive. Its really simple, evolve and innovate or accept the inevitable decline that follows.
Unfortunately GPAH explicitly excludes patients wth complex health problems. It cherry picks young, fit, well and connected patients who seldom access NHS primary care, but in doing so takes payment of these patients away from NHS GO se I Ed where they are desperately needed to balance the books to allow GP to continue seeing the full mix of patients
I’m a GP at Hand patient who suffers from mental illness, and it has been fabulous. I can see a GP within minutes, they’re super kind and respectful, always have my records read before I talk. I can get a same day in clinic appointment even in the evening. I have one GP I really like I normally see with them, the whole thing is just… amazing. Is it perfect? Nah, too much still needs done the old fashioned way. In person appointments are on a different system and don’t show in app, you need to call to request a specific doctor, a few other tiny things. But overall? It’s miles ahead of my previous two GPs!
It would be worth trying to understand how GP practices are funded, before concluding. Essentially the current funding model for General Practice cannot sustain this transformation, something needs to change
People are exerting choice based on the setting that suits their needs.
Younger healthy people of working age are embracing online consultations. As it’s convenient to them, appropriate to their condition and suits their lifestyle. The online clinician is also less likely to need to refer to notes as there will be less illness recorded and therefore with less continuity of care required.
Older people with multiple conditions, people with more complex problems o those who want to take a day off work to fit in with appointments will be able to have face to face appointments, in hopefully quicker time, due to the worried well not clogging up appointments and going online.
Universal healthcare still exists in this model. Nobody said everyone regardless of their medical condition, lifestyle needs and choice have to receive treatment in exactly the same place by the same person.
Services need to fit around people not the other way around.
Think you’ll find universal care doesnt exist with them!!!!
It’s bad practice and misleading to say everyone can sign up…..they cant, see list below.
Women who are or may be pregnant (If you are pregnant, NHS England advises that you register with a GP practice close to where you live)
Adults with a safeguarding need
People living with complex mental health conditions
People with complex physical, psychological and social needs
People living with dementia
Older people with conditions related to frailty
People requiring end of life care
Parents of children who are on the ‘Child at risk’ protection register
People with learning difficulties
People with drug dependence
Anybody would like an online consultation, doesnt have to be aged based and plenty of “young people” with the problems listed couldn’t sign up for this service
Yes it would be good to understand the GP contract e.g. how GPs make their money and why this is being held a barrier to change towards GPAH types services. Us secondary care IT types have no knowledge of that world.
If you have a chronic condition or have a medical emergency like a heart attack. Brain injury, stroke, surgery etc you can’t be seen by GP at hand, if you have signed up to them and his happens to you, you would be effectively GP_less if you were with them, and would need to find a new one
What would be easier if is these “easier patients” could use GP at hand and their regular GP reimburses GP at hand, as they are all funded by the NHS.
It’s only a video/telephone call after all with possible onward referrals and prescriptions, not rocket science!
Why can’t they all just work together?!
This is an issue with global sum and other list based funding arrangements. But try and get. GMS practice to give up their contract!
Becasue that would just be sensible 🙂
I would hope if you had one of those conditions you would be presenting at emergency care NOT your GP surgery.
So they are complaining that someone else has embraced technology where they didn’t?
Pretty sure they are private businesses…. in a market economy…. maybe this will be the kick up the backside they need to stop being complacent and look at how they can improve their own offerings.
Comments are closed.