Nine demonstrator projects are to be established across the capital as part of the One London Local Health and Care Record Exemplar (LHCRE) programme.
Speaking at a Digital Health Networks Best Practice event at London’s City Hall on 16 November, Luke Readman, CIO of the East London Health and Care Partnership and one of the prime movers of the One London bid, discussed projects designed to offer more personalised care to London’s diverse and expansive patient base.
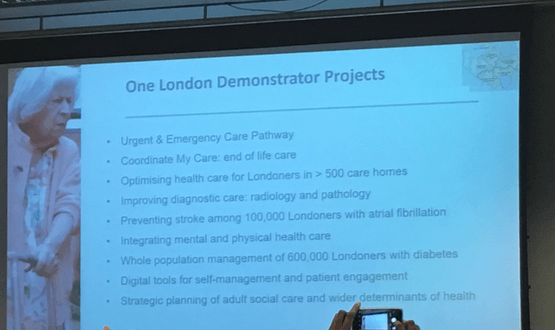
The nine demonstrator projects will cover urgent and end-of-life care, diagnostics, radiology and pathology diagnostics, stroke prevention and improving health in London, among other areas.
In one such project planned for South West and North East London, One London will deliver an integrated electronic health record system designed to enhance access at the point of residential healthcare delivery.
Care home staff will be provided with access and annotate residents’ primary care records, as well as access dashboards designed to optimise medicines management and “anticipatory” care, such as flu vaccinations.
Clinicians will be able to access records irrespective of geographies or care settings, meanwhile residents will be able to ensure their wishes in respect of urgent, emergency and end of life care.
The nine demonstrator projects were formulated with the prerequisite that each will target specific health needs of Londoners, will have measurable outcomes and can be achieved within 12-15 months.
One London demonstrator projects:
- Pan London emergency care with frailty alerting
- End of life & embedded Co-ordinate My Care providing clinical data interoperability
- LTCs: Identification and management (atrial fibrillation/diabetes)
- Care home access and communication
- Population health analytics – WSIC functionality (sharing diabetes IP)
- Roll-out of IMPARTS – mind and body interface
- Digitally engaged Londoners and self-management with PHR
- Social Care
It is hoped that data gleaned from the projects will help with the development of “learning health systems” that provide a perpetual feedback loop of data that can inform population health initiatives.
“We need to make clinical data fit for purpose for research,” said Readman.
“Then you start to drive an improvement loop that becomes very pervasive.”
As such, Readman said the One London LHCRE had settled around six “themes” for generating high-quality data.
This will include creating a ubiquitous view of data wherever patient is being seen; creating a “distributed resource of actionable data” by combining clinical data sets; exploiting opportunities to let patients link to their data, through to establishing a single London-wide approach to research data.
Readman appeared alongside key representatives and leaders from the One London network at the event.
This included Carol Dezateux, professor of clinical epidemiology and health data science at Queen Mary University in London, who explored the issues surrounding data sharing, in particular whether patients would be able to “trust an algorithm”.
Tara Donnelly, managing director of the Health Innovation Network, also spoke at the event about the innovation landscape in London.
Greater Manchester, Wessex and One London were selected by NHS England in May to become the first Local Health and Care Record Exemplars (LHCRE).
The three areas, which have a total population of around 14 million, will receive £7.5m over two years and are tasked with putting in place an electronic shared local health and care record by building on existing local work.
Thames Valley and Yorkshire and Humber were also named as LHCRE sites in June.
Over 40% of the population of England will be covered by a shared local health and care record as a result.

22 November 2018 @ 22:04
Care home staff will clutter up the GP records, making GP work harder.
Ten minutes doesn’t give much time to sort the wheat from the chaff.
23 November 2018 @ 06:59
Good point.
However if we move away moving big documents around to asking for which data you want to see. The clutter goes away – it’s the process the process that needs to change (and technology can support and enable this)
22 November 2018 @ 12:05
Hi
I think you mean 16th November quote