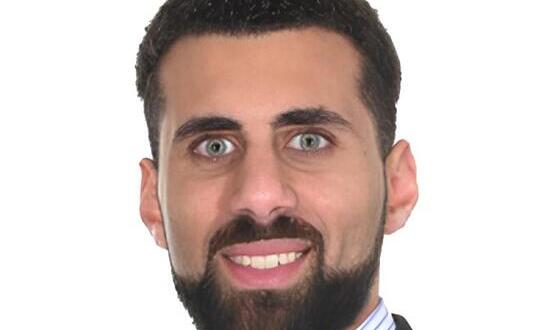
CCIO profile: Bill Aylward
- 11 June 2014

If you were to look around the NHS for an advocate of open source software and an exemplar for how it can be used by trusts, it would be difficult to look past Bill Aylward.
Openeyes – an open source electronic patient record for ophthalmic care – is Aylward’s pet project, and one he has been working on at Moorfields Eye Hospital since 2010.
The system has a wide range of functionality, covering booking and correspondence, e-prescribing, operation notes and outpatients appointments with clinical modules for specialities like cataracts and glaucoma.
One of its key features is a drawing tool that allows clinicians to easily create diagrams of a patient's eye, automatically generating a description of what has been drawn and a diagnosis.
The software is shaped by clinical input, both from within Moorfields and across the country. Groups of experts use the modules for a speciality and provide their feedback on how they can be improved to better fit their needs.
For Aylward, it is this spirit of collaboration that is key to the success of openeyes, as well as of that of open source software in general. “I think open source is a better way of writing software, because it fits how clinicians work – it’s about sharing,” he says.
Open source vs commerce
Of course, there are sceptics. At a recent conference at Moorfields, organised by EHI’s CCIO Leaders Network, a concern was raised that a trust that develops open source software will not see any financial benefit from passing it on to others; even though somebody will need to curate and support it.
On the financial point point, Aylward argues that trusts need to consider the benefits of having free access to software shaped by a range of experts.
“There are so many examples in ophthalmology – let alone outside of it – where people have contributed to the code but their trust can’t even afford to buy it. With open source, that disappears,” he says.
“If you look at it from the individual trust’s point of view, their bottom line might be less than what it was. But if there are too many proprietary deals going on as a whole, then the NHS loses money.”
Moorfields has taken a long time to get to openeyes. The trust initially piloted an in-house EPR called ProMed in 1997.
In 2000, this was handed over to a company called Target4 to develop for free in return for sales elsewhere. After some initial success, the usage rates started to fall and the system was eventually dropped.
Aylward says one reason was the stalling effect of the National Programme for IT, which discouraged trusts from paying for their own products, because they expected to receive ‘strategic’ systems from its huge contracts. “The National Programme was such a disaster, it actually held everyone back.”
It took a while for Aylward and his team to recover, but the current success of openeyes is best demonstrated by its usage rates at the hospital.
The system is used for 100% of bookings and correspondence, 60% of prescriptions, 80% of operation notes and between 25% and 80% of outpatient appointments.
Aylward says the high use of the system can be attributed to the engagement that clinicians have with the project, enabling it to be tailored to their requirements.
“It’s absolutely crucial to make sure users are involved and you understand what they want to do and make it as slick as possible.”
A friendly neek
Aylward’s passion for IT is long-held, and a topic of gentle ribbing within his family. “My daughter calls me a ‘neek’, a cross between a nerd and a geek. As soon as personal computers came out, I had one and was seeing what I could do with it.”
Aylward studied maths and computing at Cambridge University, before making a switch to medicine that was partly inspired by the large number of doctors in his family, including his mother.
“They say that if you grow up in a medical family, the world splits into two categories, doctors and patients, and you don’t want to be a patient.”
After completing his degree, Aylward went to Australia for a couple of years to complete his MD thesis, before arriving at Moorfields to study as a trainee in 1989. After moving to Miami to train in vitreoretinal surgery, he returned to Moorfields in 1994 as a consultant.
Even at that early stage, Aylward says he knew that electronic records were vital to improving the work that clinicians could do. “It was obvious then that paper was a huge barrier to patient care, research and so many other areas.”
In 2002, he took up the position of medical director and chief clinical information officer. In these posts, the issue of moving away from paper notes to an electronic system took on added resonance.
“With that agenda, things became personal. My job was to deliver improvements in patient care, get better outputs, better clinical information, and I thought this [an EPR] was the right job to get on with.”
Aylward says he is heartened by the way clinical informatics and electronic records have now become “mainstream” in comparison to their relative obscurity when he first started working within the NHS.
“Back then, it was considered a bit of an eccentric interest to enter information on computers. People had grown up with paper records: nobody was talking about a change, there was no money for it, and people just accepted it as a necessary evil.”
Now, he says there is pressure from boards and patients to move towards electronic systems – as well as from the clinicians and nurses who have grown up in a tech-friendly world.
“We’ve now got a new generation of junior doctors and nurses whose personal IT is streets ahead of their work IT. Now, everyone does everything online, so they can’t work with records on paper, they ask what’s going on?”
Making the case to the board
Aylward is no longer the CCIO of Moorfields: he gave up the role – and the board meetings – when he stepped down as medical director in 2010.
However, no CCIO has been appointed to replace him, so he is still the person most often called on to speak about informatics to the trust board.
While he has accepted the responsibility, Aylward believes trusts need a full-time CCIO to make sure that boards get an informatics perspective on the issues they are facing.
“I think that what the role brings is a care and coordinating role and a check that any informatics initiative is co-ordinated. It’s very easy for a hospital of this size to procure things without any thought about the impact on strategy,” he says.
Instead of a spot on the board, though, Aylward wants to continue his focus on openeyes: at the moment, the focus is on rolling out the software to Moorfields’ satellite sites and other trusts.
Once that is done, the project team’s focus will shift to adding functionality to the software and making improvements to assist clinicians and their patients.
“There’s a well of creative ideas for what we can do with the information, like virtual clinics, cutting down on patient journeys, reassuring patients before they even get into the clinic. But at the moment, we’re in the enabling phase.”
At some stage, there will also be an opportunity to move to a paperless system. While paper notes are still in place in the clinics, Aylward says that once openeyes is fully implemented, they can be dispensed with.
“In clinics where we have developed openeyes for the clinic, in 50% of them – three of the nine sub-specialties – the paper notes are there, but they don’t need to be. Once we finish the roll-out, which could be by the end of the year, we could simply remove them from the clinic.”
Once that happens, everybody’s eyes should be opened to the success of Aylward and his team.