Digital doctor to review NHS tech
- 30 October 2015

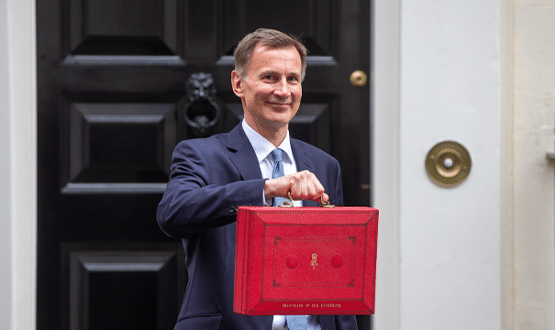
Health secretary Jeremy Hunt has announced that a best-selling US digital health author is to lead a review of the digital future of the NHS.
Dr Robert Wachter, author of 'The Digital Doctor: Hope, Hype, and Harm at the Dawn of Medicine's Computer Age' and professor at University of California, San Francisco, will “conduct a review for the NHS on the critical lessons we need to get right as we move to a digital future,” said Hunt, who was speaking at an HSJ event.
Wachter, who Hunt described as a “world expert on the promise and pitfalls of new IT systems”, has become an influential figure in healthcare IT since the publication of his book.
 |
|
Jeremy Hunt clutching a copy of the |
'The Digital Doctor', which Hunt was photographed clutching on a recent US trip, assesses the uptake, use, impact and unintended consequences of the introduction of electronic health records in the US.
Honord #NHS hlth secty @Jeremy_Hunt askd me to lead study 2 inform UK #healthIT implmntatn, inc lesons learnd frm US https://t.co/2GKauyClSP
— Bob Wachter (@Bob_Wachter) October 29, 2015
Hunt claimed the review will be comparable to Professor Donald Berwick’s work on clinical safety. “He will guide and inspire us as Professor Don Berwick did on safety and we look forward to receiving his report next summer.”
Digital Health News has asked the Department of Health for more details on how and when this review will be conducted.
The use of technology in the NHS was a strong theme in Hunt’s speech, which opened with a hip hop video made by doctors in the US about their problems using electronic health records.
He later said that, in some cases, the use of electronic patient records was seen to be adding to bureaucracy rather than reducing it.
“Whilst thanks to President Obama’s Health Information Technology for Economic and Clinical Health Act, the US has gone further and faster than most countries in digitising hospital records, this change has met huge resistance from doctors because of the extra burden that can reduce contact time with patients.”
Hunt referenced a US study where researchers took videos of 100 patient visits and found that doctors were spending around one third of the time looking at their screen. He added that another study found that emergency room doctors spend 40% of their time filling out online forms and just 28% of their time with patients.
“Put simply for many doctors it feels like screen contact has replaced eye contact.” He added: “The lesson here must be to ensure that new IT systems improve rather than reduce clinician productivity – so that it helps rather than hinders them in their jobs.”
Hunt later said the use of technology to create shared digital records shouldn’t mean that individual NHS organisations lose accountability, mentioning that problems with communications had contributed to serious patient safety failings at University Hospitals of Morecambe Bay NHS Foundation Trust and the now defunct Mid Staffordshire NHS Foundation Trust.
“We must never let shared records become an excuse for diluted accountability or the lack of a personal touch, which is why the work done by the Academy of Medical Royal Colleges about clinical accountability outside hospitals is so important.”
Other ‘elephant traps’ mentioned by Hunt for the NHS to consider when implementing digital technology include cost, stating that one of the lessons learnt from the failed multi-billion Connecting for Health programme is that incremental improvements are as valuable as ‘big bang’ changes.
The final trap is data security, with Hunt suggesting that the NHS has “not yet won the public’s trust that it is competent in protecting basic personal information”.
Despite these concerns, Hunt described himself as “unashamedly one of the optimists” when it comes to the potential for new technologies in healthcare.
He gave several examples of new technologies to support improvements in health, including microchips that can be swallowed to record all medicines a person takes; apps that can detect depression and suicidal tendencies and an iPhone attachment that can help diagnose problems with someone’s ear.
Hunt also mentioned that spirit of going the paperless ambition is “alive and well” and praised the work of NHS England to have 97% of GP practices offering patients access to their summary record online.
He concluded: “When it comes to the coming changes in healthcare, it’s not man versus machine, it’s what man and machine can accomplish together. And to that there are no limits.”