Cracking the challenge of effective clinical communication
- 24 January 2019

A recent Digital Health Best Practice Webinar discussed one of the most common challenges in modern hospitals: improving ease of communication between colleagues. Staff at South Eastern Health and Social Care Trust explained how technology has helped them overcome it. Claire Read reports.
The old surgical ward block at Ulster Hospital was what even an estate agent might have confessed was compact. “I could stand on one side of the building and, if all the ward doors were open, I could look straight through four wards to the other side of the building,” Jenny McMahon, lead nurse for the surgical directorate at South Eastern Health and Social Care Trust, reported at a recent Digital Health Best Practice Webinar.
So the prospect of moving to a new building brought excitement: staff knew they would be caring for patients in a much bigger, brighter and more suitable environment. But there was a challenge. The building has three wards per floor, with 24 single rooms, and each ward is L shaped. The days of being able to easily glance at your colleague and grab him or her to discuss a patient’s care were going to be over.
Of course, even if your colleague does generally work a few steps away from you, effective clinical communication isn’t always easy. As Steve Matarelli put it, a typical ward is noisy; staff are flooded with information; and they can be prone to alarm fatigue.
Matarelli – a registered nurse and now senior clinical executive at Vocera Communications – points that interruptions are common, and that they carry with them patient safety risks. And knowing whether your colleague is indeed just a couple of wards away or is in fact somewhere entirely different is impossible until you actually walk over (or glance through the door) to confirm – and likely interrupt.
Turning to tech
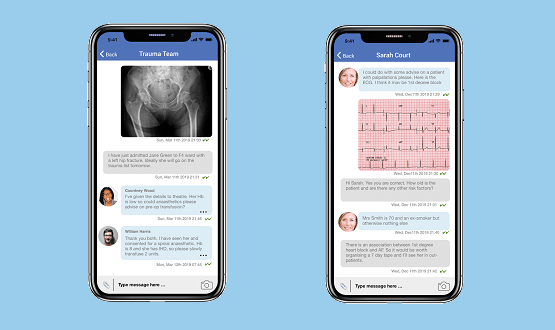
On the new Ulster Hospital surgical wards, there was a recognition that a better system was needed. They turned to a technology setup: a hands-free communication device that staff wear and through which they can talk instantly to their clinical colleagues. The Vocera Badge can also be used to locate colleagues, and a mobile app that enables secure texting also is in place to give additional flexibility.
By the time the technology was introduced on the Ulster surgical wards, it had already been implemented at the Downe Hospital. The facility was built in 2009 and according to Mark Kendall – telecommunications manager at South Eastern Health and Social Care Trust – there was a keenness to meet clinical communications needs, right from the very start. “We needed a product which was going to help us deliver a higher quality of patient care, and also meet our communication requirements.”
Intelligent communication
According to David McKee, emergency department pharmacy technician at the Ulster Hospital, it’s been mission accomplished on that front. “To get contact with the emergency department, I used to have to phone through to their landline, which if it was busy you had to stand to wait for five, 10, sometimes even 15 minutes to get a free line,” he told webinar attendees.
“And even when you got through, you didn’t necessarily get through the right person. So that was a big delay. It made me wait for something that shouldn’t be an issue. But now with Vocera I’m able to phone through to the correct person at the right time.”
Concluded McMahaon: “It’s about intelligent and effective communication, and reducing the time wasted. We need to spend all our time on patient care – not wasting time to trying to get hold of someone.”
To find out more about the experience at South Eastern Health and Social Care Trust, watch the on demand version of the Digital Health Best Practice Webinar.




5 Comments
A valuable resource that has so much potential to improve care and communication within and between teams.
Mark hawking – we are happy to share how we utilise Vocera, with some of the functions / processes etc you highlight. We are always looking to learn, to share, to develop with others!
There are two things here: the technology itself and the way in which it is integrated into the workflows in the organisation using it.
It would be very useful to have a few case studies of how Vocera has been structured . the plans produced by the organisations purchasing the technology (& whether & how the end users – all of them – were involved) and the outcomes further down the line.
Could you provide a link?
As a retired GP, it would have been great to be able to contact “the right person” in my local hospital – but had the problem that I could always be contacted when with a patient during surgery hours:patients would accept a return call: hospitals always wanted man immediate connection.
Good communications is not about good technology, it is about well designed communications processes, translated to a computing architecture and then that implemented with appropriate technology. That ‘technology’ might be a school exercise book at the side of a patients bed if that is the best way of doing it.
All this is around stated objectives, not just throwing the latest technology at what are perceived to be the problems.
It has taken me nearly half a century in computing to translate all that complexity to these simple phrases. Here it is free of charge for those who have ears to listen.
It would be interesting to hear from the clinicians involved: I can see that pharmacy would be delighted to be able to contact “the right person” in A&E instantly – and would think that saving pharmacy time was a good thing: I’m less sure that having pharmacy able to contact clinical staff busy with emergency patients at any time is equally appreciated.
There is no mention in the article of any processes or protocols – or even whether the devices have a voicemail/out of office function..
How about some information on how the tech is implemented in real life situations?
Comments are closed.