Joe’s view: Public money, public code
- 4 May 2021
After leaving the NHS in December, Professor Joe McDonald still has the health service on his mind as he looks to implement his own tech vision.
I left the NHS in December and gleefully bade farewell to some of the appalling staff side software that doctors and nurses have to use, or so I thought. A few days later I got a call from a friend in general practice to ask if could help out with the start of Newcastle’s now extremely successful vaccination programme. How could I refuse? All I had to do was three modules of training on the NHS Online Learning Management System (OLMS). My blood ran cold, I thought I had escaped the truly god-awful user interface of OLMS that is ubiquitous in the NHS.
I logged in to the mother of all UX nightmares and eventually found the required training modules and slogged my way through them, screen-shotting my end of module test results, in case the system decided to forget me or crash or have some down-time, so that I would be able to prove to the vaccination team that I knew to put the pointy end in the patient without having to repeat the experience.
Soon I had my first shift at the Vaccination Centre at Newcastle Racecourse. It was a joyous experience, many of the volunteers were recently retired and many known to me, it was a school reunion but with years of experience and a steely purpose. Within days we were a well-oiled, silver-haired vaccinating machine.
We vaccinated everything the GP record put in front of us, we found extra doses in every vial and if we had anything left at the end of the day we pulled people in off the street to make sure not a drop was wasted. This is what happens when you in-source a healthcare problem to the NHS and give NHS people the resource to get the job done. Yes, I am looking at you, Test and Trace.
Open source revolution
At the same time as my nasty, and I hope final, encounter with OLMS, I got a call from Kevin Monk, CEO of SARD JV, the small company who provided appraisal software for myself, a rare example of usable back office software for NHS staff with instant online support, so he had my attention. No, I am not on commission.
“Would you like to help us with an open-source revolution in NHS software?”
“Errrrr, no thanks Kevin. The NHS isn’t interested, there’s a cosy duoply in primary care and we’re signing long contracts for American EPRs in secondary care. We lost that war largely without firing a shot and we are cementing in our proprietary foundations. Covid-19 made it even worse, the NHS is now fully addicted to Microsoft Teams.”
“But, Joe, you preach the gospel of a modular, cultivational approach to health tech espoused by Prof Margunn Aanestad? You applied those principles successfully in The Great North Care Record, right?. OK, the game may be over in the EPR market what about all the misery caused by staff side software, that wastes NHS time and money too.”
Of course he’s right, the EPR is just one of many systems deployed in an NHS trust and I have been obsessed with them to the exclusion of all the other systems. This is a genius idea! What if you could get the NHS to move to an open platform, cultivational, modular approach on the staff side of the NHS, by sneaking around the back of the expensive monolithic EPR with a SUS [System usability scale] score of 52, rather than a full frontal assault on well-dug in and treasured deployments upon which a generation of CIOs and CCIO’s have bet the farm. A bit like the closing scene of Independence Day when Jeff Goldblum and Will Smith infect the alien invaders’ mother ship with a viral payload that spreads and saves the earth.
Eventually it might even enable EPRs to be interoperable and modular. A radical idea but one worthy of a trial I think. Like the vaccination campaign, in-source NHS IT, starting with staff side software.
The grand plan
But how? Well, Kevin and I are both fans of Matt Hancock’s 2018 tech vision, and his reiterated desire at Rewired recently to separate data and applications shows an understanding of these issues which we are unlikely to see again in a secretary of state for a very long time, if ever. So we need to act now and somewhat impertinently, we have taken taken it upon ourselves to write a Tech Vision Execution Plan. You can read it here.
Central to that plan though is the creation of a company, Public Money Public Code Limited (or CIC, or co-op or whatever), to develop staff-side systems that are designed to be modular and interoperable.
Having watched the NHS try to procure its way to modern interoperable health tech fruitlessly for the last 15 years, it’s time to try something else. For too long the NHS has turned up at the dogfight of the health tech market without a dog. We need a dog in the fight. In cognitive behaviour therapy we say “if you always do what you’ve always done, you’ll always get what you’ve always got”. With the news that NHSX is to be absorbed into the new transformational wing of the NHS alphabet surely now is the time to do something genuinely different.
When George Osbourne gave me £4million, as part of his Connected Health Cities initiative, we built The Great North Care Record which was used nearly a quarter of a million times last month.
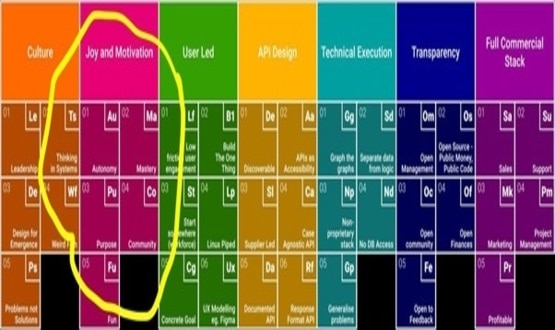
If Matt Hancock gives me £5 million we will deliver Public Money Public Code Limited and show how to execute his Tech Vision. Not just in terms of code but also all the other periodic table of essential elements required to breed success, the culture, the community, the soft stuff that made Great North Care Record a success.
As we say in the North East, “Shy bairns get Nowt.”
Declaration of interest: Joe McDonald has done some paid consultancy for SARD JV but his and Kevin Monk’s work on the Tech Vision Execution plan is unpaid and there is currently no budget identified for a tech vision execution plan.





9 Comments
Helpful!
Dear Joe,
You seem to be enjoying yourself enormously in your retirement. But you have unfinished business. Your Great Health Care Record made it possible for hospitals, GPs and even social care to swap patient data more or less seamlessly up there. But down south, we can’t.. And to make it worse a conversation I have been having in these pages in the past few weeks (“three strategic tech priorities….”} have persuaded me that there is no will, leadership or expertise down here to achieve any widespread interoperability,as you did in the North.
Your tech vision sounds promising – although I am too old and frail to understand what you mean by ‘cultivational.’ Can you please come out of retirement and bring the South into the twenty first century. Your country needs you
And what about all the patients in the North? Do they all have access to THEIR DATA?
Too kind Richard. Rumours of my retirement are somewhat exaggerated. I have retired as an NHS Employee and therefore enjoy the freedom to speak plainly without the fear that many inside the NHS feel if they want to voice any criticism of central NHS bodies governing NHS IT. To speak up is to jeopardise your NHS Trust’s chance of gaining funding for innovation. This toxic atmosphere of patronage is at the heart of much what is wrong with NHS IT and it doesn’t look much like changing anytime soon. Given that , I think it is for us as a community to attempt to bring about the culture change we require to unleash the true power of NHS data. You can start by following @PubMoneyPubCode on twitter
Oh dear, , Public Money, Public Code looks good but too long-term to be ready in my lifetime. Particularly as the culture of the NHS is still Trust-centric and ‘bottom up’ – not a good environment for integrated care systems. In my part of the country, there has been zero progress towards interoperability in the last twenty years.
R YOU sitting comfy (*) then i will comment, i agree with joe, as things stand at the moment, it makes far more sense if public software is developed in the private sector … why ? there is a significant leadership problem (*) in many of (y)our PS organisations, shame … as the UK has some epic software developers !!!
there are massive (& significant) problems within the NHS, many of them to do with the tech, but just like europe, the best way to sort problems is from within not being on the outside, this approach may drive a person mad but i believe it is the right thing to do. NATIONAL vaccination has been a massive success, the NHS has played it’s part, but so have many other PS and PS organisations. MY BACKGROUND IS TECH, THAT IS WHAT I HAVE BEEN TRAINED TO DO AND THAT IS HOW I HAVE EARNED MY MONEY ! the NHS needs to create more career pathways for techies and not PUSH them down a managerial route … the NHS, or more precisely, the PEOPLE working within the NHS, must sort itself out !
NHS Digital should be NHS National, does that make sense?
If you want to contribute to the tech vision execution plan please join us here
https://publicmoneypubliccode.org.uk/
Comments are closed.