To realise their potential all virtual wards must be tech enabled
- 11 April 2024

In the first of a two-part series on virtual wards, Tara Donnelly examines evidence of “excellent” progress and explains why there is much more to do on tech enablement
It was fascinating to be part of the establishment of the virtual ward model during the pandemic, and to watch it scale across the NHS in England. Every ICS now has this service available for its residents.
Importantly, we now have good data on the progress of virtual wards from national data returns and from large scale public surveys and can draw a number of insights from these.
Public appetite for a more home-based, tech-enabled model of care appears to be very strong across the country – and it is older people who are most keen to use tech to stay out of hospital. One of the main myths that persists about digital home care is that older people won’t like it, or be able to use it, but the evidence is quite different.
They are also the biggest group being cared for on virtual wards. The Health Foundation undertook a large survey last summer of 7,100 people and found that the vast majority – 78% of people of all ages – would be happy to monitor their own health at home using technology instead of in a hospital. Among those aged 65 and above, this rose to 85%, the highest score from any age group.
Progress to date
Throughout this column I’ll be using statistics from the most recently published National Virtual Ward SitRep (situation report), which came out in January 2024 and covered the period to the end of December 2023. While the data quality is not perfect, it is the best we have in illustrating the national picture.
This demonstrates that 332,742 people have been cared for at home rather than in hospital since May 2022. Virtual wards are now running at a healthy 73% occupancy and almost 15,000 people experienced this care on the NHS in December 2023.
Most patients benefitting are doing so due to admission avoidance, (47%), or early discharge (35%).
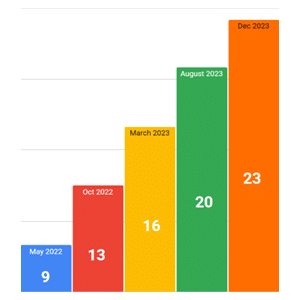
In May 2022 there were nine virtual ward beds per 100,000 population; the most recent count at December was 23 beds. When you consider that there are around 250 physical hospital beds per the same sized population, according to OECD benchmarking, this means an extra 9.2% capacity is now being provided by virtual wards. This is all new capacity, built over the last four years, as before April 2020 none of this existed.
The vast majority – 75% – of those cared for in a virtual ward in December 2023 were over 65. As children’s virtual wards begin to develop, we are starting to see some volumes in the under 16s, now 6% of beds. The remaining 19% are between 16 and 65.
It is excellent progress in a short amount of time and the change in clinical pathways is impressive, as we all know the tech is the easy bit of any major transformation.
Areas for action
However, there is much more to do on tech enablement. Remember, part of the core NHS definition of a virtual ward is that it must be tech enabled; that is, as well as contact at home from nurses, doctors and other professionals by phone, video and in person, there needs to be remote monitoring technology enabling the patient to share vital sign and other information with their care team.
While most – 59% – of virtual wards say they are tech enabled, the national return indicates that less than one third – 29% – of patients in December actually received this model of care.
It is important to maintain the momentum on virtual wards, to continue to grow the services to reach more people. The overall ambition is to reach 40-50 beds per 100,000 population and this would mean moving from 9.2% of the bed base (as measured against the OECD stats) to 16-20% of it. That would be a major achievement, and while the specific virtual ward funding block ended at the end of March, there is a larger, recurrent urgent and emergency care pot for ICBs to use to maintain and increase their virtual ward provision in the future, as outlined in the recently published NHS Planning Guidance.
To realise their potential, virtual wards all need to be tech enabled, so that their care can truly be described as equivalent to hospital care where National Early Warning Scores (NEWS) can be readily viewed, and patients reassured or escalated based on objective data of how they are doing.
Encouraging feedback
It is great to see expansion of digital home care into new settings beyond virtual wards, with trusts using this technology to support people at home from same day emergency care, on waiting lists and to help them better manage severe long-term conditions.
It is also hugely encouraging to see the emergence of very positive feedback on virtual wards from patients. One of my clients is Doccla and in addition to conducting the usual patient surveys, they’ve recently started asking people who have tried virtual wards if they would mind filming themselves answering questions about how they found it. They’ve rapidly built a great collection of feedback from people sharing what a difference this model of care made to them. Linda’s feedback – “it was marvellous!” is typical.





