Working together and using digital health to tackle disease
- 7 December 2021

Chris Sawyer, the innovation lead for digital Health at Innovate UK, explores how small and mid-size enterprises (SMEs) and the NHS can work together and use digital health to tackle disease.
There is an African proverb I love that says: “If you want to go fast, go alone. If you want to go far, go together.” During the last four years, I have been lucky enough to witness some amazing people working together in health that have transformed the sector faster, further and more fairly than ever before.
The secret of this success is the ambition of digital innovators, who know that our health service can be stronger and it can work better for patients. So by connecting these individuals and companies with the right people, insights, knowledge and expertise then great things can happen.
Most people think that UK Research and Innovation (UKRI) is all about funding. But probably the most important part of our role here working on the Digital Health Technology Catalyst is to inspire new collaborations. Because funding can only go so far if an idea isn’t fit for purpose, or work for the patients or clinicians it’s designed to help.
Especially in health, innovators have to navigate complex, often fragmented processes and systems. This can take time and waste energy, resources and dilute their ambition. The right connections however can accelerate how quickly and effectively a new idea is developed, tested and adopted in the real world.
Collaborations can take many forms and have many different benefits. To show the richness of partnerships happening in digital health at the moment, I want to share five great stories with you today, so you are as inspired as I am about how impactful we can be when we work together.
1. Tapping into sector specialisms
Great collaborations are so often about bringing in specialisms that you don’t have within your own team or to get deeper expertise that will ensure an idea is fit for purpose. Daysix is one of our funded companies that is developing The Trauma App to assist in major trauma cases and record critical patient data, with the aim of transforming the effectiveness of trauma care to ultimately save lives.
This exciting Edinburgh-based digital software agency already has a great track record in health, but it knew it needed to turn to the Scottish Trauma Network to help tap into its expertise. Working with representatives from Scotland’s four major trauma centres and EmQuire, a group of clinicians at the Queen Elizabeth University Hospital in Glasgow, Daysix was able to ensure its digital tool met the current trauma protocol and included all the necessary insights that trauma teams would use in real-world scenarios.
2. Testing technology in the real world
Technology is only as good as the benefit it has. We only know the benefit of these great digital health technologies when we test them in the real world. Oviva has found a way to help people who have Type 2 Diabetes take control of their weight loss. Its self-management digital lifestyle tool has the potential to support safe but rapid weight loss helping patients lose 15kg in 12 weeks and then maintain that for life. But Oviva has only been able to know this for sure when it trialed its innovation with 250 NHS patients from South West London and Buckinghamshire, following them up to 24-months. The trial is being independently evaluated by the University of Westminster and Insight Health Improvement so that Oviva can evidence it delivers at least the same or superior patient access and clinical outcome benefits as current face-to-face support models.
3. Making sure ideas are patient-led
Patients should be at the heart of all our ideas. If our funded technologies don’t improve outcomes or increase standards of care then we’re not fulfilling our mission. Family Mental Wealth is building its app, Headway, almost entirely on patient insights – some of them deeply personal ones. After supporting their own daughter through childhood mental ill-health, Nick and Carol Pollard wanted to help other parents. So, with their daughter Dr Elizabeth McNaught, who is now an NHS GP, they designed an app that combines the clinical know-how at King’s College and Maudsley Learning with input from families who have very real, lived-experience of childhood mental ill-health. The hope for Headway is that these rich patient insights will ensure the app is relevant in the way it helps parents identify signs of mental ill-health and provide them with evidence-based techniques to help their child build a mentally healthy life.
4. Pivoting technology from – and to – other industries
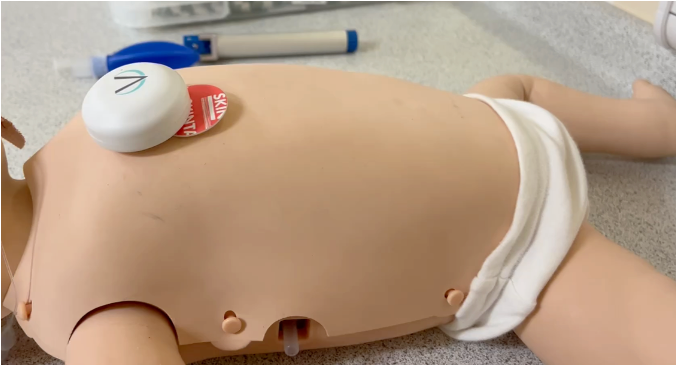
Looking to other sectors will help us develop ideas in health and show how they can be adopted at scale. Generic Robotics has blended cutting-edge software with approaches already used in the eLearning industry to address the shortfall of trained healthcare personnel and help reduce the strain on the NHS. Its clinical simulator, SimuTouch combines haptics (technology that can create the experience of touch) with sensors and virtual reality to help test the capability of newly qualified doctors. By standardising training and recreating real-world test scenarios, SimuTouch has the potential to assess thousands more doctors, saving the NHS time and money. We’ve been able to help Generic Robotics not only develop the technology but collaborate with expert medical educators at King’s College London to help it scale. Importantly for the UK, this technology has the potential to pivot into more industries such as Energy, the Arts, Construction or Manufacturing.
5. Smoothing the way to get new ideas adopted
Any innovator doesn’t want their idea to fall at their last hurdle which is why collaborations can be key to market access. Big Health has developed Sleepio, a safe and effective non-drug alternative for poor sleep and insomnia that not only helps people recover from insomnia but could save the NHS money and free up already-stretched clinical resources. This kind of technology falls into a relatively unexplored area of digital self-help within the NHS which can make it more challenging to secure uptake from the NHS. This is why Big Health has been collaborating with the NHS and the Oxford Academic Health Science Network to explore reimbursement models to ensure the service can be prescribed and directly referred to by healthcare professionals.
Smoothing the way
Whether it’s about exploring if an idea is fit for purpose, developing it with the right insights, testing a prototype or, indeed, getting it into the hands of the right customers, collaborations are vital. Going it alone can be, well, lonely but it can also require much more effort, time and resources – and can be at times a dispiriting place to be. Collaborations smooth the way, add huge value and strengthen the chance of your innovation being adopted at scale.
We would encourage any innovator out there with an ambitious idea about how our health system – or indeed any system – could be improved to reach out and find good partners to come on the journey with you. And of course, the teams here at UKRI and the funds we offer are set up to help you go faster and, importantly, go further.