Five things to watch in primary care, 2014
- 2 January 2014
Health secretary Jeremy Hunt has electrified the healthcare IT industry with his call for the NHS to go ‘paperless’ by 2018, but many GP practices have been paperless for years.
This means the hot topics in primary care IT for the coming year are not what systems to install or how to get them used effectively.
Instead, the themes for 2014 will be how to move forward with a new GP Systems of Choice contract, how to give patients access to their records and other services, and what is going to happen to GP information as NHS England pushes ahead with the care.data programme.
On the commissioning front, securing information for commissioning and dealing with the implications of Dame Fiona Caldicott’s second report on information governance in the NHS are also likely to feature heavily.
Jump to read:
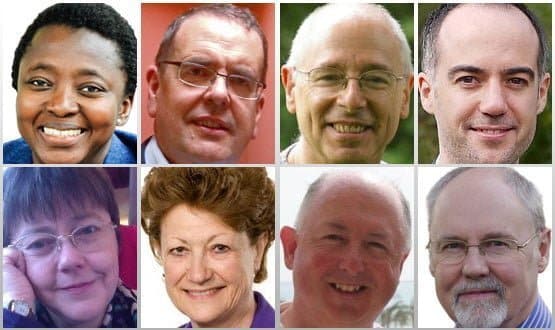
- Kemi Adenubi on GPSoC2
- Ewan Davis on GPSoC2
- Dr Brian Fisher on patient access
- Geraint Lewis on care.data
- Julia Hippisley-Cox on care.data
- Dame Fiona Caldicott on Caldicott2
- Dr Alan Hassey on the use of PCD in commissioning
- Dr John Lockley on PCD for commissioning
GPSoC2
GP Systems of Choice is a framework contract that funds GP IT systems for nearly 80% of practices in England. The Health and Social Care Information Centre is in the midst of procuring a new GPSoC framework that is due to be signed by March 2014. This involves significantly more suppliers and a range of new features.
Kemi Adenubi, GPSoC programme director, says: “The arrangements in the new framework are geared towards helping practices get the best out of their GP clinical IT systems.
"User specified roadmaps and incentives for suppliers to improve the utilisation of national services – such as the Electronic Prescription Service and the Summary Care Record – which are aimed at developing an increased focus on good training and continuous improvement of delivered software.
“The new framework will establish a transparent route for third party suppliers to interface with GP clinical IT systems, [if they] meet information governance and data protection requirements, and will include funding for some key services that may be delivered by third-party systems, such as appointments management and clinical decision support.
"Practices will be able to choose services to be paid for within a funding envelope and will also be able to fund additional services from their local budgets.
“Based upon a strong model of identity management, the new GPSoC framework will also offer patients access to a choice of online services, including access to their GP record and booking appointments online and asynchronous communications with the practice staff.”
Ewan Davis, co-founder of the Healthcare App Network for Development and Innovation (HANDI), says: “GPSoC2 is a welcome step but its effectiveness in opening up systems will depend on the extent to which the Health and Social Care Information Centre can make sure that principal systems are held to their contractual requirements and how quickly we can progress to richer and more standard interfaces.
“Responding to the pressures on primary care to improve quality and access against a background of increasing demand and restricted resources will require a radical change in the nature of general practice.
"GP IT will need to be able to respond in an agile way to the requirements that will flow from the changes and the heavyweight structures of GPSoC are unlikely to facilitate this.
“In the medium-term, we will move away from institutional records to patient-centred records making the concept of a GP system as we understand it today obsolete and irrelevant. A GPSoC2 that locks us in an old paradigm is not likely to facilitate this process.”
Patient access
The promise to provide patients with access to their online records by March 2015 has been repeated any number of times by health secretary Jeremy Hunt. However, the nature of that access has been quietly trimmed back just as often.
EHI revealed in October that the minimum GPs will have to achieve by this date is to provide patients with access to the information in the Summary Care Record. The new GP contract, which comes into effect next April, also ties them into providing online appointment booking and ordering repeat prescriptions.
Dr Brian Fisher, London GP and founder of Patient Access to Electronic Records Systems (PAERS), and the winner of this year’s John Perry prize, says: “Its two steps forward and one back.
“[On the positive front] GPSoC has been mandated to fund patient-facing services for the NHS, while the Patient Online programme is exploring a number of key issues that need to be in place if record access is to work, including information to the public and support for practices.
“A third positive is that the big beasts of EMIS, TPP, INPS all offer record access now to varying degrees in their GP IT systems.
"The plan is that all their application programming interfaces will become open for smaller providers to offer record access through all of the principal providers – that offers a vital route to success.
“However, there are gloomier aspects. The BMA has fought a rearguard action and has ensured that key support and policies have set back opportunities for patients, practices and the NHS to benefit from record access.
“So, the direct enhanced service for practices to offer record access has disappeared and the minimum definition of record access has been watered down. That doesn’t prevent suppliers from offering more sophisticated versions, but it may mean that practices will be resistant to anything other than the basic SCR proposition.
“Hopefully, it will be patient demand that drives the funding and the process. Patients will want more – and maybe some practices will too, once they see the benefits coming through.”
Care.data
The care.data programme involves taking a large monthly dataset from all GP practices covering patient demographics, events, referrals and prescriptions. This will be linked with Hospital Episode Statistics and other datasets to create new Care Episode Statistics.
Datasets from care.data will be available publicly in aggregate form and in pseudonymised form to commissioners and health researchers. GP extractions are due to start in March with linked datasets available from June 2014.
However, the programme has been beset by rows about the usefulness of this approach, and the consent and confidentiality issues it raises.
Geraint Lewis, chief data officer NHS England, says: “In 2014, GP and hospital data will be linked for every patient in England. For the first time, commissioners will be able to analyse outcomes, compare services, and identify unwarranted variations in care nationwide.
“We think that patients and providers will be reassured to know that there will now be evidence to underpin planning decisions, particularly those relating to integrated care.
"Another first is our sending a leaflet to every household, informing patients about how their health information is used beyond direct care to benefit patients.
“NHS England is committed to transparency and we want to ensure that patients understand the importance of health information in improving the NHS as well as the choices they have over the use of their data.
"GP practices will continue to play an essential role in raising awareness and in providing balanced information so that patients can make informed decisions.
“Finally, we will work with the GPES Independent Advisory Group to ensure that researchers and other approved analysts can access the pseudonymised linked dataset to bring more benefits to NHS patients.”
Julia Hippisley-Cox, professor of clinical epidemiology and general practice, Nottingham University, says: “There is enormous potential for using GP data for research and generation of public benefit. However, there are some unresolved issues to address before the public benefits of care.data are likely to accrue.
“These include: transparency for patients on the use of their personal confidential data; how best to maximum use of privacy enhancing technology to protect patient confidentiality; and the utility of the proposed extract.
“Care.data may lead to a profound change in confidential doctor-patient relationships since information will be routinely shared with the HSCIC and others.
"Concerns have been raised that care.data may undermine public trust in doctors. This could leave patients uneasy about disclosing clinical information relevant to their care.
“There is a small window of opportunity for NHS England to address the outstanding issues and make best use of privacy enhancing technology whilst maximising the public benefits of care.data. We could then look with more confidence to what might be the data equivalent of the industrial revolution.”
The second of Dame Fiona Caldicott’s reviews of information governance aimed to balance the need to keep confidential information confidential with the need to share it across health and social care teams and to use it for research.
The Caldicott2 report, issued in April, introduced a new ‘duty to share’ information where it is in the best interest of the patient.
Dame Fiona Caldicott says: “The security and use of health data has steadily risen up the political agenda since I was asked to review information governance in 2012, particularly the balance of protection and sharing of patients’ health information.
“This year our independent review was published and its 26 recommendations accepted by the government. We called for a culture change where IG is concerned and much greater attention to sharing data in the patient’s interest. The Secretary of State for Health also asked me to convene a new independent panel to scrutinise and challenge progress in those recommendations being implemented.
“As we enter 2014, there is a platform in place from which the difficulties of commissioning in particular, and the use of health data for research and public health, have been clarified in terms of current law and regulations. After much work by many people in the Department of Health, NHS England and the Health and Social Care Information Centre, numerous problems have been resolved.
“So I anticipate that my new panel will be able to facilitate the improved use of people’s information for their care, especially at interfaces in clinical pathways, but also for research, enabling patients to participate in that when they wish.”
Patient confidential data flows
Primary care trusts were able to use a Section 251 exemption (from the provisions of the NHS Act 2006) to access patient confidential data in order to complete some key tasks, such as population risk stratification and invoice validation.
However, these powers were not transferred to the new clinical commissioning groups when PCTs were disbanded in April 2013.
At first, this looked like an oversight. But when the second of Dame Fiona Caldicott’s reports on information governance came out, and the Department of Health responded, it became clear that the government meant to clamp down on the use of PCD for this purpose.
This means commissioners must navigate a new way of working in 2014 without regular access to PCD, but this is no easy task.
Dr Alan Hassey, senior clinical advisor, Health and Social Care Information Centre, says: “We want to see the five patient confidentiality rules we set out in our 2013 ‘guide to confidentiality in health and social care’ become part of the DNA of all those working in the system.
"As the vital new Caldicott principle puts it: “The duty to share information can be as important as the duty to protect patient confidentiality."
“[However], other aspects of the second Caldicott review will have major implications for our work, including the need for commissioners to have a proper legal basis for their activities.
"The HSCIC is establishing a Caldicott Implementation Monitoring Group and one of its key tasks will be to help bust myths and anxieties that have grown up around the use of PCD to support commissioning.
“We will be working with NHS England and commissioners to find answers for risk stratification, and invoice validation, and a solution for establishing accredited safe havens [centres where information can be held].
"The thread running through all of this work is putting the patient and the service user firmly at the centre of all considerations.”
Dr John Lockley, GP, clinical commissioning group member, and CCIO Leaders Network columnist, says: “In the past, some PCTs were too liberal over access to PCD – but the pendulum has now swung too far in the other direction.
“Most patients assume that their personal medical information will be shared with other healthcare professionals who need to know it.
"I’m sure that patients also accept that this sharing of information needs to extend to checking the accuracy of the financial aspects of their care under the NHS. In a sensible world, all this would be performed using the NHS Number.
“At the moment, we are all facing the ‘Call to Action’ to save £30 billion of NHS money.
"Yet under the Section 251 debacle, CCGs have been deprived of the ability to do it, because they aren’t allowed to view the identity of patients seen in hospital. It’s been like trying to balance the books when the paperwork is held in a permanently locked safe.
“Meanwhile, at the same time that NHS England is interfering with CCGs’ access to PCD, it is insisting that copies of PCD held on all GP systems should be sent to the HSCIC under the care.data project without any of it first being anonymised or pseudonymised. Where is the consistency here?”




