Advisory Series: Portals
- 16 June 2017


Portals – Advisory Series, June 2017

By Claire Read – Digital Health
In the second of Digital Health Intelligence’s new advisory series, Claire Read looks at how sustainability and transformation plans are embracing portals – and considers how the concept is evolving.
It’s a simple word, but ‘portals’ has a remarkable ability to polarise opinion in health IT. It’s fair to say Ciaron Hoye isn’t a big fan. “I absolutely hate the term,” admits Hoye, who is head of digital at Birmingham CrossCity Clinical Commissioning Group. He fears it is a “very vanilla description” which immediately conjures up an outdated understanding of its meaning.
“A lot of people when you say ‘portal’ think, ‘oh, right, a web page’,” he argues. “Well, no. That’s a very nineties and noughties idea of a portal.”
The Amazon model
Certainly, the sort of functionality which take centre stage in Birmingham and Solihull’s STP is a long way from the likes of Yahoo! or CompuServe or Lycos.
Hoye, who co-authored the area’s local digital roadmap (LDR), prefers comparisons with the likes of Amazon. He wants portals to be the means of putting patients in control, and for them to offer a truly single point of access to information drawn from all the services with which citizens interact.
“It’s about giving that kind of experience to patients, and changing the social contract between care recipient and care provider,” he suggests. “So let’s look at Amazon and say can I have a single digital front door, and then a range of things behind it?
“Can I put 10, 20, 30 portals behind a single entry point? That’s what Amazon Marketplace does. So what if we took concepts like that which have already been used elsewhere and apply it to healthcare.”
Uniting primary and secondary care
At present, the area has two well-developed patient portals: myhealth@QEHB and MyHealthcare. The former gives individuals with long-term conditions access to their records, results and letters from University Hospitals Birmingham Foundation Trust. The latter covers 23 GP practices in Birmingham and enables patients to electronically book GP appointments, see their GP notes, and request repeat prescriptions.
Both will be developed further as part of the local area’s digital plans. It is hoped patients will soon be able to use myhealth@QEHB to consult with their healthcare professionals. In primary care, meanwhile, the aim is to have patients using the portal to give – or refuse – consent for various groups to access their records.
But the biggest aim? To bring primary and secondary care together. “We’re exploring whether we could put access to both systems behind a portal,” explains Hoye. “Effectively, could we have a portal which accesses both portals? Then we’re getting to [a patient] being able to access their holistic care.”
The need for portal interoperability
It’s an idea strongly supported by John Uttley, e-innovation director at Midlands and Lancashire Commissioning Support Unit. “In some areas where a patient portal is being bought – and this was previous to STPs coming together in the way they’re working now – there is the potential you might end up with a solution where a patient needs to have access to multiple portals in order to see the totality of their record,” he suggests.
“We talk about interoperability for clinical systems, and there needs to be an interoperability standard for integrated care records, for patient portals.”
Certainly, there is unlikely to be a shortage of such systems. In Digital Health Intelligence’s 2017 NHS IT Leadership Survey, the full results of which will be published at the end of June, half of respondents spoke of shared health and care records as a major current project. A quarter named clinical portals as a current area of focus.
Uttley helped write the local digital roadmap for Shropshire, Telford and Wrekin, an area which neighbours Hoye’s patch. An existing clinical portal is named as a key digital asset in the plan, which also details a desire to develop a patient portal.
“We want to have a portal for patients to access their clinical record, to update their record, to give consent and to see who’s accessed their record, and it would be based upon their joined-up record,” he explains.
Evolving definitions
Purists, of course, would say portals simply involving bringing information from disparate sources into one read only view. Interaction may not traditionally have been the name of the portal game, but Uttley firmly believes it must be now.
“To me, unless you’ve got something which is going to be interactive, that adds value to the patient, then I think it’s going to be a waste of money. For me as a patient, I would want to interact with my record so I could update it – I should be able to send information from FitBit around what my sleep has been, or information around my blood pressure.”
It again speaks to the idea of portals as empowering people to deepen their understanding of their own health and how best to take care of it.
Patient empowerment
It is a theme echoed in Norfolk and Waveney’s plans. In this area of East Anglia, a prototype integrated care record has been built with a view to improving patient and GP access to information.
“It’s part of a range of measures about supporting patients to stay well in their own homes, offering GPs the flexibility to support patients away from practice settings, and also ensuring the sustainability of services,” reports Geraldine Wingfield-Hill, programme director for Connected Digital Norfolk and Waveney.
“I think the added dimension that it can bring to how we deliver things is patient empowerment, and enabling self-care to come much more to the foreground,” suggests Simon Cooke, a GP principal at Norwich’s Oak Street Surgery, and the chairman and chief clinical information officer of local GP alliance OneNorwich.
“I think so often we see patients who are very much in a health helplessness sort of state. And their anxiety drives a lot of their symptoms, and it’s really based on not knowing and not having confidence in the knowledge they’ve got. Very often when you illustrate to that patient where they are in life, and what their metrics are, it just enables them to have confidence in themselves, and that then enables them to build more resilience and robustness in themselves.”
Driving sustainability
It’s a big role for a portal – nothing less than driving the sustainability of healthcare. Not that Wingfield-Hill says the prototype has much to do with the original understanding of such a setup anyway.
“Behind it, there’s a single database and the prototype presents a number of different views of the data, including data which is anonymised. It can do more than a traditional portal,” she says.
It is another point in favour of Hoye’s argument that the term portal is now somewhat inadequate; poorly reflecting the full range of functionality which could be involved.
“If you look at our local digital roadmap in Birmingham, Solihull and Sandwell, there’s a consistent piece around communication and collaboration,” he says.
“Communication is at the very heart, and if the portal becomes a channel for communication in both directions – it can be how I tell you something, it could be how you tell me something – you open up some really interesting possibilities.”
Shifting communication, citizen empowerment

By Servelec
Today, we can access and manage a wealth of sensitive information online such as our bank accounts and utility bills. Increasingly, people expect the same level of access to be available to information in support of individuals’ health, personal care and wellbeing.
Health and care services are looking at new and innovative ways to redesign their services to empower people to manage their support needs online. A new model of cross-enterprise collaboration is emerging in the sector, where an online portal enables multiple stakeholders to access an individual’s health and care data. This includes being able to view summary care record information as well as contribute to assessments and care plans online.
For care services, the benefits of shifting communication, engagement and transactions to digital channels have helped to improve and speed up the user experience, enabled better use of resources and improved outcomes.
From the individual’s, and their carer’s, perspective, having real-time access to the information held by care services is empowering and supports informed and shared decision making.
Sharing information, improving care
At Servelec, we believe in a joined up approach – sharing information, improving care.
As health and care services continue to join up, our vision focuses on a collaborative community-based approach, providing modern innovative systems and portal solutions that support the delivery of care to the right people at the right time wherever they may be. Our focus is to integrate service areas into one single digital pathway that will bring greater efficiencies and savings. Our offering:
- improves access to information
- delivers cost benefits
- increases productivity
- delivers time savings – data is only entered once and is available to a number of systems
- supports effective decision-making and timely interventions
Finestra is our innovative portal solution that offers a platform for citizens, young people, carers, parents or representatives, to manage their information and contribute to their care and support online. Professionals and providers from other agencies can also use Finestra to view and contribute to a record online. Finestra offers:
- a rich environment for publishing information, advice and guidance, self-assessment tools and personalised information output
- forms that are fully integrated with Servelec’s electronic patient record solution, RiO, and Mosaic, our leading social care case management solution which enables users to provide information once and allows updates and contributions to their record
- a marketplace enables a user to manage their personal health budget, as well as to commission and pay for services
A person-centred approach
The personalisation agenda is transforming how the NHS empowers patients and is one of the key ambitions of the NHS Five Year Forward View. The Forward View sets out a shared vision for the future of the NHS in partnerships with local authorities and local communities for a better future.
Self-directed support enables individuals to have more choice and control over their care, and develop the knowledge to be able to take an active role in the management of their care. Transforming the relationship between people and their health and care professionals into a true partnership, laying the foundations for achieving improved health and wellbeing outcomes.
In working towards this shared vision, Servelec is positioned to deliver the ‘big picture’ single view with our best of breed solutions from across our suite of leading software and portal solutions for health, social care and early years/education management. We believe this approach enables all stakeholders to access the information they need to improve outcomes for themselves and the people they support.
Finestra supports person-centred planning and a self-service approach enabling individuals to manage their care and support planning, personal health budget and commission services. The shifting of communication and engagement to digital channels enables individuals to access and engage with care and support services more effectively, providing them with the ability to be in control of their own information.
Health and care services need business intelligence to manage delivery and identify service gaps or trends that deliver improved outcomes for the community. Our business intelligence tool, Corius, offers added value by providing integrated reporting and dashboards, gathering data from across the suite of Servelec’s software solutions (or other systems) providing both a comprehensive view of the current picture and a forward view to help identify and interpret trends.
Our person-facing solutions support personal health budgets building on a decade of experience supporting people in social care to manage their personal budget. Our innovative budget management tools, available 24/7, enable individuals to manage their budget, and commission and pay for support services through online transactions. Our solution also uses a role-based access security and permissions matrix that enables full access control to everyone involved in a person’s circle of support.
Delivering a single view strategy for children’s services
Integrating services is essential to providing a single view of a child’s journey through the health and care services. Finestra supports children, young people and their families to work in partnership with practitioners, by providing access to appropriate parts of their record in Mosaic and to input directly into their ongoing plans and reviews. This also meets a key Ofsted objective to provide evidence of the voice of the child in their case record.
Being able to monitor their child’s education, health and care plan on Finestra allows parents to understand what support is available and being delivered. Parents can also update the plan with all the services. Having one shared plan covers the child’s needs more comprehensively and this integrated approach allows all the support services to understand the big picture for each child.
In adoption and fostering services, foster carers and adopters can use Finestra from the moment they wish to express an interest in becoming a carer; through the recruitment and approval process and once they are approved. The portal provides them with the ability to update their own record as well as the records of children and young people they are caring for.
On the early years and education management front, our Synergy solution offers purpose-built portals for professionals, parents/carers, schools and service providers and each offers dedicated tools to support the tasks they are required to perform. This includes; applications for school places, free school meals, and free early education places for two-year-olds, school admissions list rankings, early education ‘head count’ processing and self-service directory listing updates. All of these activities involves interaction and engagement from a range of stakeholders; from parents, schools, local authorities, childcare providers to service providers. Each activity is proven to save significant time for local authorities, as these tasks would otherwise have to be performed manually.
For all stakeholders, embracing the shifting of communication and transactions to digital channels and being able to self-serve 24/7 is key to the digital agenda. Contact us today to find out more about how we can support the enhanced delivery of your services.

|
|
| Contact number: 012 4643 7573 Email: servelechsc@servelec-group.com Our website: www.servelechsc.com Twitter: @servelechsc LinkedIn: www.linkedin.com/company/servelechsc/ Further reading: Finestra – the innovative portal to empower social care Care Settings [ssba]
|
|
5 steps to a successful Integrated Digital Care Record project

By Orion Health
Orion Health is the UK’s largest provider of clinical portals, or Integrated Digital Care Records. By an IDCR we mean a system which can integrate a citizen’s health and care data from disparate systems across a geography into a single view. From this single view clinicians and care givers can then utilise additional functionality such as care planning, test ordering and referral management. In our 15 years’ experience partnering with NHS organisations, including the multi-award-winning Connecting Care programme in Bristol, we’ve seen common themes in the most successful projects. Here are our top five tips for ensuring that your IDCR project thrives:
In our 15 years’ experience partnering with NHS organisations, including the multi-award-winning Connecting Care programme in Bristol, we’ve seen common themes in the most successful projects. Here are our top five tips for ensuring that your IDCR project thrives:
- Get the right project leadership – Securing a strong project lead who can provide continuity and a clear vision is perhaps the most defining factor of a successful IDCR implementation. They need to be effective in uniting stakeholders across all the participating organisations that may not have a track record of working together. It is also essential to have a strong steering committee with clinical and local authority champions to support and help drive change management.
- Develop compelling use cases and track benefits – This is crucial for getting stakeholders and end users on-board right from the start of your IDCR project. If people can’t see the real-world value they’ll get in return for changing their workflows upfront, you’ll likely struggle with engagement throughout. Set a baseline to enable benefits realisation at the start of your project, including data points such as average bed days, access times and patient experience. You’ll then be able to track and prove results down the line.
- Remove barriers to uptake – A primary measure of a successful project is user uptake. The most successful projects we see have been careful to streamline user workflows as much as possible. Minimising the number of clicks to access and avoiding the need for multiple system log-ins is key. Orion Health can facilitate single-sign-on with GP systems such as EMIS to optimise user experience and encourage adoption.
- Release functionality in phases – Portal projects are complex, from juggling data challenges to accommodating requirements for a variety of user roles. Avoid trying to do everything at once and take an iterative approach, focusing on the most valuable features first and progress along a well-defined and agreed roadmap in phases.
- Surface the right information for the right users – When you launch your IDCR, if users don’t find the information useful the first time they log in, you’re unlikely to get a second opportunity to capture their interest. We have a ‘top 14’ list of data items we recommend to help organisations to avoid this pitfall. It’s also beneficial to configure role-based views of the portal to cater for different users, a social worker will need to see a different view to a GP for example.
Follow these steps and you can deliver a successful IDCR which delivers better ways of working for clinicians and care givers, improved patient experience, cost and time efficiencies and more. There are now a number of vanguards who have already been through the process of launching an IDCR, so making reference visits and knowledge sharing along your journey can both inform your own plans and bolster confidence. To learn how Camden Clinical Commissioning Group have successfully developed their Care Integrated Digital Record, and to find out more about Orion Health’s solutions, click here.
* 23.1% of the UK Clinical Portal market, Digital Health Intelligence May 2017

|
|
| Contact number: 087 0486 8406 Email: emea-marketing@orionhealth.com Our website: www.orionhealth.com/uk/ Twitter: @OrionHealthEMEA LinkedIn: www.linkedin.com/company/orion-health/ Facebook: www.facebook.com/orionhealth/ Further reading: NHS Camden CCG Health and Social Care Northern Ireland [ssba]
|
|
Western Health and Social Care Trust: Cross-Border Integrated Care IT Solution

By Karen Carty and Gina Naughton – RIS/PACS team Galway University Hospitals, Saolta University Healthcare Group
Under starter’s orders
Implement a safe, secure and easy to use integrated ICT solution to allow sharing of clinical images between hospitals in Saolta University Health Care Group, Republic of Ireland, and Altnagelvin Hospital, Northern Ireland.
Across-border radiotherapy treatment project has been setup to enhance patient comfort and care and will enable patients from County Donegal in the Republic of Ireland access radiotherapy services at nearby Altnagelvin Hospital, Northern Ireland.
This will reduce the patient’s travel time on treatment days from seven hours to 40 minutes. Clinicians in Altnagelvin Hospital need real-time access to the up-to-date radiology record of patients attending for radiotherapy treatment. This will facilitate effective patient review, multi-disciplinary meeting discussions, treatment planning and follow-up.
On your marks…
An estimated 500 cases from the Republic of Ireland could be treated in Altnagelvin with potential for 1,000 cases per annum for review, as not all will go on to have treatment. The solution has to ensure that only data on patients who have given consent for their data to be shared will be made available to authorised clinicians in Altnagelvin Hospital. A tight timeline to go-live for cross-border project meant the solution had to be up and running within six months.
Get set….
After a review of the available solutions, Agfa HealthCare’s Integrated Care Suite was selected as Galway University Hospitals were already using the XERO universal image viewer. This functionality was extended within the Health Management platform, enabling healthcare providers at Altnagelvin Hospital to access and display patient data in real-time, without needing to move or manage it.
Go…
Phase 1:
Secure sharing of images/reports by manual push from PACS to Portal
Download of data from Portal to local PACS also available
Phase 2:
Full integration between PACS systems, with;
DICOM integration
Study availability notifications
Report integration
Role based access control and authentication
Winner!
This is an integrated care model providing benefit to patients, their families, carers and clinicians. The ability to integrate and interoperate with other systems has always been important to Galway University Hospitals radiology staff, having implemented the first paperless/filmless radiology department in an Irish public hospital in 2005.
“We have witnessed an increasing demand for image sharing between public/private hospitals, cross-border and even worldwide. We continue to move with technologic advancements creating integrated care solutions ensuring our patient’s clinical data is available when required at the point of care. This project is a prime example of what can be achieved when hospital personnel collaborate and work together with the technology available to them.”
This project took less than six months from project initiation to Phase 1 go-live and proves that…
“Who Shares Wins”

|
|
| Contact number: 084 4892 2004 Email: paul.jackson@agfa.com Our website: www.global.agfahealthcare.com/main/integrated-care/ Twitter: @AgfaHealthCare LinkedIn: www.linkedin.com/company/agfa-healthcare/ YouTube: www.youtube.com/user/agfahealthcarevideo Facebook: www.facebook.com/Agfa-HealthCare Further reading: Radiology and Electronic Patient Record Electronic Radiology Record [ssba]
|
|
Beyond patient portals: Opening a window on citizen engagement

By Dr Justin Whatling – Vice President, Global Population Health
Prevention is better than cure. It’s an old adage, but one that still rings true today, not least within health and care, where being connected makes all the difference to both providers and individuals.
Activating communities in their health and care is imperative to a better experience and delivering the IHI triple aim. We are supporting providers across the health system with the technology to do just that.
Rather than placing the citizen at the centre of the care process, we advocate that people should be active members of their own care team, and engaged in wider aspects of health and wellbeing – a goal shared by the NHS Five Year Forward View. This way of thinking is integral to shift from a system of reactive care to one of proactive health, with data being combined to securely create insight that can help you to know your citizens, engage them and manage their outcomes on an individual, organisation or population level.
Connectivity is at the core of this, as it is in modern life generally. People are more than happy to buy food, order taxis and do their banking online or through apps, yet healthcare finds itself lagging. Patients still face difficulty accessing services and understanding their own medical details – contributing to poor management of long-term conditions, non-attendance and unnecessary bookings.
People, not patients
The future will rely on people being empowered in their own health so that, ultimately, they don’t become patients at all. Health is 24/7/365, not just when a health and care professional can see you, so providing the tools, support and information required to stay healthy is key.
The Five Year Forward View advocates providing citizens with both clinical advice and access to their medical record and history, empowering them to manage their own health and giving them more control and choice. Where many strategies consider a patient portal to connect patients to their care, Cerner is looking beyond this with HealtheLife® – a citizen engagement platform built to support an individual’s holistic health.
Changing attitudes?
Users are already confident enough to directly share personal fitness data with hardware providers like Apple and Fitbit, suggesting a thawing towards how people feel about their data as the Internet of Things takes shape. If there is a personal benefit to be had, without compromising security, individuals will be interested.
It’s the job of the health and care economy now to assure citizens of the benefits and ensure that their data is protected. It is our job as suppliers to ensure that these do not become new disconnected islands of data, but that they contribute to the same single source of truth and allow citizens to engage as a member of the care team.
Secure, available, usable
Through HealtheLife, individuals can actively engage in their care by securely accessing their information and messaging their care team, including attachments such as pre- and post-visit questionnaires. Video calling from within the platform, currently being piloted by our clients, allows care providers to monitor treatment plans and intervene before problems occur, and help reduce unnecessary appointments.
People are online, and healthcare must be too. HealtheLife can be accessed on smartphones, tablets or desktops, allowing access at any time of the day or night. It also means that individuals can access relevant elements of their own medical records, or those of an approved family member. Accessible elements include lab results, documents and clinical notes, radiology and pathology reports, medications, allergies, immunisations and procedures.
There is also a full repository of educational and motivational material – to engage people on lifestyle choices, such as those surrounding smoking, drinking, immunisations and exercise.
The importance of interoperability
Being interoperable and open is a crucial part of this change. HealtheLife can connect to data across your health system and be fully customised to suit the needs of your health system and users, whether they want an easy way to schedule appointments, or have proxy access to help a child or elderly person manage their medications.
We’ve built HealtheLife to be compatible with third-party developers, meaning that more widgets and greater usability can be added, to ensure that you can deliver the best experience for your communities. We connect wearables and other smart health devices so that the data can contribute to medical records and population health programmes to support proactive or prescribed health, care and treatment goals. Whatever the future holds, HealtheLife will be ready and functional.
HealtheLife in action
Wirral University Teaching Hospital NHS Foundation Trust is one organisation that is utilising the benefits of HealtheLife and is the first in the UK to pilot the solution for maternity and diabetes. Having had a successful integration, the Trust’s CEO David Allison, believes that individuals can now “take a greater part in their care and be more engaged in what they have to do as a patient and a partner with the clinical team”.
Now is the time when the patient is can be empowered to actively manage their health and wellbeing, and the health system is able to understand and leverage big data and advanced intelligence to help keep people from becoming patients.
Cerner’s health information technologies connect people, information and systems at more than 25,000 facilities worldwide and our clients are using our population health platform to proactively manage the health of almost 100 million citizens. To discuss your vision and how we could help, email cerneruk@cerner.com.
|
|
| Email: CernerUK@cerner.com Our website: www.cerner.co.uk Twitter: @CernerUK [ssba]
|
|
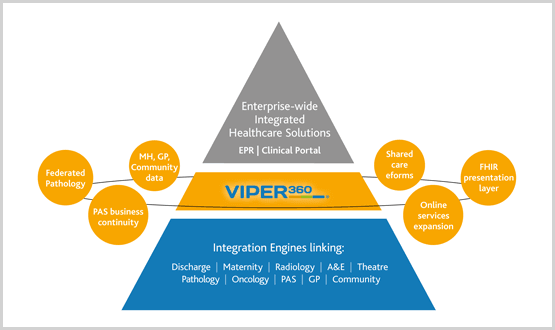
From Portal to Interoperability Platform
By Mike Symers – CEO, Restart Consulting Ltd
Until recently, the view was that large-scale enterprise-wide integrated healthcare solutions would assist NHS organisations to move up the Digital Maturity Index. Healthcare portals are still deemed a key component of this development, however, as budgets are being further constrained, fewer of these major investment projects for healthcare exchange solutions are now coming out to tender. Trusts, local authorities and CCGs are all looking for innovative ways in which they can better utilise their existing digital assets/budgets and get more functionality out of their Integration Engines. Recognising this position, NHS England’s Interoperability Handbook, published in September 2015, advocated the use of open technology as a way of increasing the number of suppliers in this market place, and as an alternative to proprietary systems.
As this market develops, there is still a lack of solution providers in this interoperability space, which exists between the top end functionality provided by the enterprise-wide solutions, and, the lower level functionality provided by the integration engines within trusts. In between these two sets of capabilities, ReStart has identified a real opportunity for agile solutions to help organisations get more out of their existing systems. We see this opportunity increasing in proportion to the waning of appetite, and budget, for large-scale and complex multi-stakeholder portal decisions.
ReStart provides integration services and support to over 70 trusts and this is a space we really understand well. With this background we have taken the decision to invest in a presentation and interactive layer solution – Viper360®. The goal is to step into that interoperability solution gap between enterprise-wide solutions, and the trust integration engine, to give healthcare providers a building-block approach to integrated healthcare. This approach will support a trust’s aspirations to move up the Digital Maturity Index, starting from a low-cost base.
With its modular, open-technology approach, Viper360 prevents data duplication. By providing real-time access to clinical data, Viper360 is offering concise clinical information at the point of view. The Viper360 vision is built on providing three layers of functionality, each representing greater Digital Maturity to its users.
Level 1 is a view-only presentation layer suitable for early adopters of integrated healthcare.
Level 2 provides an interactive layer with read/write back functionality.
Level 3 provides clinical pathways developed for the local healthcare economy.
Hugely flexible, Viper360 can be used for shared healthcare plans, workflows, and patient portals depending on customer requirements, with completely configurable screens and data flows. Viper360 represents a versatile solution platform currently being rolled out at a number of sites.
Examples of these projects are:
In South West Yorkshire Partnership NHS Foundation Trust, Viper360 is delivering a county-wide project to bring historic patient data into one place, and provide real-time access to current and legacy community, mental health and acute data in a single user-specific view.
In Nottinghamshire Healthcare NHS Foundation Trust, Viper360 is being used to link disparate patient administration systems from mental health, psychological Therapy, community and primary care systems. It provides clinicians with full access to patient records, and maximises the opportunity to place a patient on the correct pathway at the earliest opportunity.
In Derby Teaching Hospital, Viper360 has been deployed as a business continuity solution to ensure system-based patient admissions, transfers and discharges could continue to be managed in the event of planned, or unplanned Lorenzo PAS system downtime.
In all its applications Viper360 has been adopted to help organisations access current and historic data on patients across different systems, to streamline service provision and to make clinical decision-making safer. In its deployments, ReStart takes a phased approach from proof of concept to full roll out across major multi-site and multi-service providing Trusts. Viper360 projects are also scalable starting from £100k proof of concept (with initial benefits delivered within six months) to £500k full-scale deployments, depending upon complexity.
Viper360 accesses existing data sources and makes it available real-time, with clinician specific views, and across the full health environment that a CCG or STP needs. Viper360 delivers many different solutions with real-time access such as:
- Acute, mental health, GP, community data presented in single patient record
- Shared care eForms
- Cross-community alerting
- FHIR presentation layer
- Federated pathology platform
- Online services expansion
Yes, Restart can deliver a portal, but that isn’t all Viper360 does. Any system that can be integrated to present clinical information via Viper360 can form the basis of an integrated healthcare solution. That makes this solution flexible, speedy to deploy and affordable. The landscape is changing and ReStart offers an innovative solution in this new interoperability market place.
| Contact number: 084 5680 3249 Email: sales@restartconsulting.com Our website: www.restartconsulting.com/ Twitter: @RSConsult_UK LinkedIn: www.linkedin.com/company/restart-consulting-ltd/ Further reading: Press Release: Nottinghamshire Healthcare NHS Foundation Trust Case Study: Derby Teaching Hospitals NHS Foundation Trust [ssba]
|
|