Hunt to promise every NHS patient app access to records

Health Secretary Jeremy Hunt will say every patient in England should be able to use an app to access their medical records and book a GP appointment by the end of 2018.
Hunt will on Tuesday say in a speech at NHS Expo that by the end of 2018 all patients should have access to an “integrated app” to access NHS 111, view their health record, book a GP appointment and order repeat prescriptions.
The promised app, expected to be the latest incarnation of the NHS England development NHS.uk national patient portal, should also enable patients to “express their organ donation preferences”, “express their data sharing preferences”; and access support for managing a long term condition.
In a Department of Health press release Hunt said: “People should be able to access their own medical records 24/7, show their full medical history to anyone they choose and book basic services like GP appointments or repeat prescriptions online.”
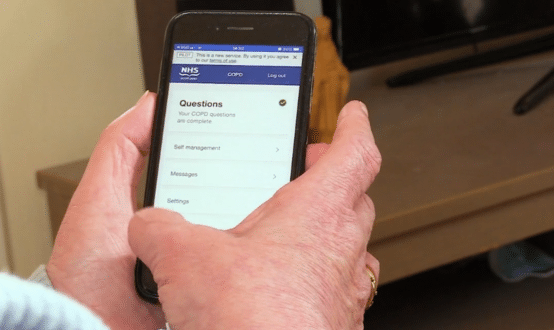
Pilot schemes are already underway including an online trial in South East London where patients can access NHS111, book GP appointment, order repeat prescriptions and receive online consultations with their GP using a mobile app.
The DH said online trials of support for long term conditions have also been highly successful, with apps such as MyCOPD supporting patients with managing their condition independently. “The ambition is that this level of digitally led treatment should be available universally.”
However, past efforts by the Department of Health to develop compelling official apps and digital patient services nationally have met with decidedly mixed success. They have often struggled to win over public and patients, while repeated attempts to establish a curated library of NHS approved ‘safe’ apps have been mired in red tape.
Much hinges on the launch of the redeveloped NHS.uk later this month, which and is intended to provide a national portal to digital patient services, including personal health records.
In recognition of the rapid growth of a range of independent commercial digital services, some of which have received critical recent CQC reviews, the Department of Health will launch a consultation about which further areas could be included in the CQC’s ratings system.
And showing an enduring commitment to the value of open data, the Health Secretary is also expected to launch the MyNHS open data challenge, a £100,000 fund, which will reward the most creative and innovative apps and digital tools making use of our open data to generate new insights that help to improve services.
Sarah Wilkinson, chief executive of NHS Digital said: “We welcome the Secretary of State’s clear vision for the provision of technology services which will empower citizens to access NHS services and manage their health. Good digital services will make care safer and more accessible and free-up more time for doctors and nurses to spend with patients.
“We are already working intently towards the delivery of these outcomes and have made substantial progress, in areas including enhancing 111 Online and NHS.UK and launching acute and mental health Global Digital Exemplars. She said NHS Digital was “ committed to achieving the targets outlined by the Secretary of State, by the end of 2018″.




20 Comments
Here we are, a month after Jeremy Hunt and Sarah Wilkinson unveiled what is needed to put the patient on top, with apps all feeding into the GP’s EPR. But I am still waiting for somebody to explain to me in words of one syllable – because I am an elderly patient with very little brain – how we are going to get from where we are today – which is not very far – to where they want to get to.
As this discussion here has made clear, a lot of silos up and down the country have gone part of the way already. How are these pioneering initiatives going to be melded together into a borderless seamless “national” system? Or will they be binned, and started all over again.
I ask, because two singing-and-dancing earlier national initiatives, Connecting for Health and care.UK, went down the Swanee after years and millions had been wasted, just because no one had thoroughly thought out the strategy. I have a nasty feeling the same will happen here.
I’m afraid I don’t trust any data banks to keep info safe – security is a huge issue. I also do not want my data sold on to every Tom Dick and Richard Branson. I’m happy to share with the NHS only. No private company should make money out of patient data.
I understand, but we do urgently need medical researchers to be able to analyse patient info (anonymised) . That is the only way we will get new drugs etc. That is eminently possible using current technology to protect patient identifiable info.
However , I certainly want very clinician delivering my care to know ‘ who has done what and when’ to me. That is critical to deliver integrated care.
He’s just headline grabbing , like making NHS paperless. What’s being proposed goes back before Grainger when we last had SHA’s I seem to recall, so I won’t be holding my breath for anything to appear.
Richard (and Jeremy Hunt as well):
Apps are already here and have been for years. I have offered online access to GP records, appointment booking and repeat prescription requests for years (thanks to EMIS). Patient Access, Evergreen Life etc.
1) Most practices allow one-way communication, i.e. you can email your practice (not necessarily your GP). Two-way communication is perfectly feasible, easy encryption is available ( http://www.tinyurl.com/NHSencrypt )
2) Many hospitals are trying to minimise snail mail, but not every patient is digitally enabled, and hospitals are years behind GP in IT
3) You can do all that now
But for 4), and all of the above, it comes down to the willingness of clinicians to do any of this, given the enormous pressures of workload (particularly for GPs) at the current time.
Yes Neil, you are a “smart” GP, but many of your colleagues aren’t. Mine is quite smart, (and uses EMIS web} but has not implemented everything I would like. It is a post-code lottery, depending, not on the availability of the technology, which has been around for oincks, but on the willingness to abandon ancestral ways of working. I do agree, however, that GPs are miles ahead of hospitals.
Neil,
It would be useful if someone could publish a map of the whole country showing all the silos where GPs, hospitals, other bits of the NHS, AND PATIENTS, are seamlessly linked together. The map should show the size of the silos. For instance my GP surgery is part of a minuscule silo, where only one local hospital is linked to it. (Hardly a silo at all.) Joe’s Great North silo on the other hand is immense.
My bet is that the majority of the GPs across the UK are not in any silo at all, despite the technology, as Neil says, having been there for years. I hope I am wrong, as patients are at risk when GPs are not connected – and patients cannot see their records.
ANd I’m agreeing with you. I’m just saying, lets ask loads of patients what they actually want. And then build that.
It’s going to be a lot of what you said.
Don’t disagree with that but are NHS England or Digital that close to the patient they can do that?
Maybe they should listen to what trusts and business wants and support them. maybe that is defining open apis to use, standardising them and let the coal face do the apps.
HI Richard,
I think that is the problem. patients are not front and centre in this plan. Unless that changes any ‘strategy’ will ultimately fail.
(sorry to be a doom monger ..
Has any one asked patients what they want? And I mean patients who don’t work in Digital Health before you reply to this comment with your “we need APIs” ideas.
I am a patient, and I do not work in Digital Health, but I can tell The Insider what I want. For starters:
1. To communicate with my GP and other bits of the NHS by email or Facetime.
2. For hospitals to abandon snail-mail altogether.
3 To be able to see on my GP’s website test results, letters to/from my GP/hospital, discharge summaries, referral letters. I would like to correct mistakes in the data.
4. For GPs to use health apps as a diagnostic tool.
However, what I want is not neccessarily what every patient wants. Patients come in many shapes and sizes. Some, with long-term conditions need more than this, maybe Telehealth. Others “keep away from quacks” on principle. Others pursue damaging lifestyles with enthusiasm, and the the last thing they want is to see their medical record. I suspect that the majority of patients are like that.
However, we are where we are: with lots of silos of varying sizes. Jeremy Hunt and Sarah Wilkinson have to decide pronto whether to link all these silos together or tear them all up and start again. I suspect that they have not thought seriously about either option.
There are still to many silo’s of information in the NHS. NHS staff don’t have access to full patient information (whether through portals or otherwise)
I think its currently unlikely that patients will get any meaningful access to their data any time soon (unless of course Jeremy has some magic fairy dust to sprinkle).
Throwing money at this wont help – what is need is a very clear patient record strategy.
The intentions are correct, however GPs will not make more appointments available online than currently. How is this any different than patient access and systemonline, which seem to be doing everything Hunt is talking about already?
Fantastic stuff but we still have not digitised medical records so might be a bit of challenge…a bit of case of “cart before horse” I’m afraid Jeremy…
We have a donkey, some wheels and sellotape with GP systems.
We should start there and build up rather than wait for perfection before we do anything.
Fifteen years ago, I cheered when Richard Granger, the NHS IT Czar,launched Connecting for Health, whci was to link all GPs and hospitals electronically.
So far, in 2017, all I get electronically on my GP’s website is blood-test results from one of the three hospitals which treat me. I can also, with difficulty, book an appointment two weeks ahead with one of the GPs.
So what magic is Jeremy Hunt going to use to do the rest of things he promises in the next 16 months?
There is only one thing the NHS needs to be doing and that is exposing underlying APIs to patients so they can easily and readily access their data and use with apps and services they choose.
The current portals, data downloads and other such wasted efforts offer little if any value to most beyond appointment booking and basic transactions. We need to enable the whole of the healthcare industry to engage. We need to empower individuals.
Nice
API’s API’s API’s Zzzzzzzzzz!!!! API’s are not the issue! they are available through GP Connect! and a huge number of providers – an integration interface (Yes integration! NOT interoperable) is the issue – and how likely is it that you’re going to get a GP supplier to develop one with you especially when they now have their own product!
Comments are closed.