Ashes to ASHs
- 19 September 2013

The use – or non use – of patient confidential data has become a key concern for GPs in their new role as NHS commissioners.
When primary care trusts were axed and clinical commissioning groups created five months ago, the section 251 exemption of the NHS Act 2006 that PCTs had used to handle PCD for a range of planning, business and targeting activities was not transferred to CCGs.
At first, this looked like an oversight. However, Dame Fiona Caldicott’s second review of information governance, which has just been accepted in its entirety by the government, said that PCD should only be used for ‘direct patient care’.
Commissioners, their commissioning support services, and the businesses trying to work with them, are complaining bitterly about this, with some commissioners saying it has left them unable to fulfil their statutory duties.
However, the government’s response is resolute, saying: “The [Department of Health] agrees with the review’s findings that health and care commissioners should be able to meet their objectives without compromising patient confidentiality or public trust in the health and care system.”
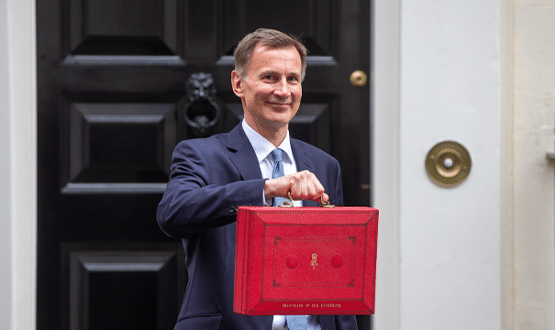
At the launch of the response last week, health secretary Jeremy Hunt acknowledged that the current situation has led to “some problems on the ground”, but said the DH would be publishing more guidance shortly.
“I think the rules are fine. It’s just that the way we are implementing it at the moment has run into some difficulties, and we have to crack that. I can’t tell you an exact date,” he said, adding that: “It won’t be months.”
A workable change?
The DH says a team from the Caldicott review worked with representatives of a local health economy and the NHS Commissioning Board [now NHS England] to determine why there were calls for access to confidential data by NHS commissioners
The panel identified seven types of commissioning activity for which access to PCD might be required, but “gained assurance from the NHS Commissioning Board and from PCT representatives that most of the challenges could be overcome in other ways, without using confidential data.”
The government’s response acknowledges that maintaining business continuity in the new commissioning environment has been a challenge, even without the added requirement of moving from using PCD as the norm to using pseudonymised or de-identified data.
“It is not surprising, therefore, that many commissioners are not yet convinced of the feasibility of using de-identified data for commissioning purposes, particularly given the increasingly personalised nature of commissioning and its role in supporting integrated care,” it says.
Work in progress; action now
Convinced or not, it looks as if they are going to have to get used to the new world. Dame Fiona recommended that ‘accredited safe havens’ should be established to give commissioners access to weakly pseudonymised data for some commissioning functions. This would probably involve use of the NHS Number.
In April, NHS England was granted a six-month extension to a Section 251 exemption to allow some identifiable data sets to be disclosed by the Health and Social Care Information Centre to CCGs and CSUs working towards ASH status. This expires on 31 October.
All CSUs and some CCGs have expressed an interest in becoming an ASH. However, the DH response does not directly endorse this solution; saying only that an information governance sub-group of the Informatics Services Commissioning Group will consider the creation of ASHs.
“In the meantime, NHS England is working on short-term solutions for those activities where there is an urgent need for identifiable data, and the department is consulting with members of the ISCG information governance sub-group so that this work is considered in the wider context of the whole health and care system,” the report says.
NHS England is also “working with the HSCIC to review systematically the data needs of commissioners and to identify options for how these needs might be delivered without recourse to using identifiable data.”
This review will “identify areas in which the HSCIC will need to develop additional capacity and capability to process personal confidential data under its powers, as well as any outstanding issues that may require long-term statutory support.”
Dr Steve Kell, co-chair of NHS Clinical Commissioners, welcomes the work and Hunt’s promise that a permanent solution will not take months, but says: “Commissioners need action now.”
He adds: “This is highly complex and until solutions are developed CCGs will continue to be unable to deliver statutory functions.
“Our members continue to raise issues of concern about this with us and NHSCC will persist in advocating on their behalf to the DH, NHS England and the HSCIC until a satisfactory solution is found.”
David Stone, NHS South London CSU’s head of information governance also broadly welcomes the Caldicott2 review, especially in areas where, “the NHS has not always been as clear as it should be on how or why data is being used”.
“However, we believe more work needs to be done to ensure that the legal distinction between health records and care records is understood and the impact this has on sharing data in multidisciplinary teams spanning health and social care.
“Being clear is important, especially where we are supporting projects to introduce integration between health and social care providers, alongside the CCGs we work with. We wish to rapidly adopt the recommendations, but it remains important that we also recognise the immaturity and complexity of the new NHS landscape, something that the report does not do in all cases.
Stone comments that some of the wording of the government’s response suggests watering down of the ambitious recommendations, for example, “… the Department will be looking to deliver the spirit of the review, rather than confine itself to the recommendations”.
“We hope that this will be clarified as soon as possible so that we can provide the best support to our customers,” he adds.
Ignoring industry
Anthony McKeever, chief executive of MedeAnalytics, tells EHI that the line between a doctor acting as a clinician and a doctor acting as a commissioner is very fine and so, therefore, is the line between clinical and administrative use of data.
While he believes the bulk of Caldicott2 makes a lot of sense, he says: “There haven’t been any answers to the practical questions yet; these issues affecting commissioning are the ones that worry me.”
He also feels that “the NHS appears to be over-complicating things in some ways. It’s not looking for pragmatic solutions. It’s inventing its own rules and approaches instead of relying on the rules and the methods that apply to everything else.
“I consider it to be both essential and in the public interest that commissioners should be able to do their job properly. And just like the CCGs, I don’t think they necessarily can if they are denied the tools to do their job.”
McKeever adds that while the NHS is normally inclusive in terms of asking industry experts for advice, neither his company nor any other companies he is in contact with were involved in the review panel that looked at issues of access to PCD.
Neither has he seen its final report. He is also concerned that only NHS organisations appear to be being offered the opportunity to become ASHs.
“My understanding is that ASHs are what comes next, but the process for getting there is somewhat mystical and very partial as it appears the only people that can apply for them are those with the letters CSU in their name,” McKeever says.
The other view
Not everybody is unhappy, though. Phil Booth, co-founder of medConfidential, a campaign fighting for confidentiality and consent, says there are some “fine words” in Calidcott’s report and the government’s response, but he wants to see some “rapid progress” on the recommendations.
He describes it as “lamentable” that PCTs and now CCGs and CSUs have relied on Section 251 exemptions for secondary uses, and is pleased that a line is being drawn under their doing this.
“We should not be conflating administrative or commissioning services with the direct care of individuals. Of course there will always be some administration, but Caldicott itself just did not accept that PCD was required for that sort of purpose.
“If they are genuinely trying to improve information governance in the NHS, then they should be using anonymised data and people need to be properly informed about exactly what secondary uses are being made of their data.”
No going back
The DH response and Hunt’s words mean the PCD tap will remain firmly turned off for commissioners.
It is up to NHS England and the HSCIC to come up with workable solutions for the NHS to continue to function without PCD. Who will bear what may be a significant extra cost of these work-arounds has yet to be seen.
The implications of Caldicott2 will be explored at EHI Live 2013 in a new stream: ‘Information sharing – making Caldicott2 work.’ EHI Live 2013 is a two day conference and exhibition at the NEC in Birmingham from 5-6 November. This year’s conference is free for all visitors to attend.