Building the Business Case for a CCIOs
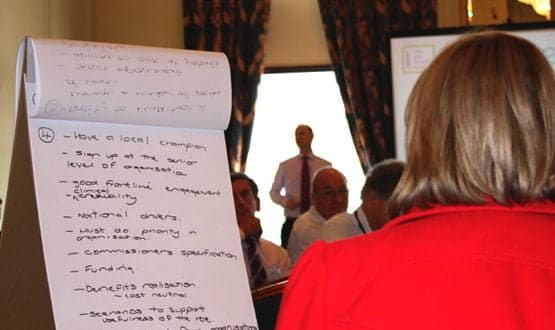
Building a convincing business case for CCIOs and similar roles is a significant challenge, to help stimulate debate and share ideas the EHI CCIO Leaders Network and the Clinical Health Informatics Forum ran a dedicated workshop in Darlington in June.
Attended by over 50 clinical information leaders from across the North East the event tackled the thorny questions around how to build a robust business case for CCIOs.
The morning began with scene setting presentations from Dr Jonathan Richardson, chair of CHIF, followed by Jon Hoeksma, editor of EHI. Bill McAvoy Deputy Transition Director, Patients and Intelligence, NHS Commissioning Board then offered a national perspective followed by Dr Daniel Birchall, clinical information lead at Newcastle University Hospitals NHS Foundation Trust, who described how his trust had built an infrastructure to support clinical information leadership.
A facilitated workshop session then broke examined four related questions
1. How do you begin to build a local business case for a CCIO?
2. What are the financial arguments for appointing a CCIO?
3. What are the clinical arguments for appointing a CCIO?
4. What is needed to make a compelling local business case for a CCIO?
The lively workshop provided a rich vein of suggestions and thoughts on how to begin building a business case to appoint a CCIO. A summary of the points is given below:
1. How do you begin to build a local business case for a CCIO?
Developing a business plan
• Costs required
• Implementation plan
• Understanding the strategy
• Implementation plan
• Understanding the strategy
• Baseline current state of organisation
• Gather evidence – lessons/benefits to other organisations
• Align to local and national best practice and business needs
• Governance very important
• Learning from others (through networks)
• Project management structures
• Close gap/align between shop floor and management interactions, local and national strategy
• Creating a strategic view and links in the organisation
• Successful model in the US that can be looked at
• Can’t be done on the hoof – need to set time aside for this work
• Ask the what if question… Look at and review something that didn’t go well…and ask “would a CCIO make a difference?”
• Service implementation
• Improved outcomes for patients
CCIO skills and development
• Build links to education providers. Improved workforce skills
• Make sure that information is seen as a key to service/organisation future and structure
• Focus on the role of clinicians leading interpretation
• Engaging clinical staff and information teams
• Business = healthcare and so leaders need to understand the business of healthcare
Focus on leadership
• Executive sponsorship is essential
• Clinicians best placed to be leaders – by framing business in terms of clinical issues/outcomes and to improve
• Transformation/change leadership
• Looking at national picture and the context
• Having some influence internally and externally in our organisations
2. What are the financial arguments for appointing a CCIO?
• Better control over developments
• Less wasted time/resources
• Clinical relevance and efficiencies
• Reduction in estate
• Supports ‘smarter’ working
• Clinical information (structured) entry creates business information
o Transactional
o Efficiency (same job better)
o Effectiveness (do a better job)
o Competitive advantage (better outcomes, better planning and better cost control)
• Strategically important (investment not a cost of doing business)
• Hope it would help reduce waste
• Clinical engagement
• Patient safety aspects
• Helps provide patient focus
• Monitor and CQC to achieve targets
• Viewing pathways across multi organisations
• Maximising the benefits
• You get more for your money – clinician/health informatics
• Ability to multi task
• Reduction of litigation costs
• Less duplication of data entry (which can account for 20% of nursing time)
• Transport costs, medical records library costs
• Stream-line operational processes
• Efficiencies
• Less waste i.e. purchasing
• Patients outcomes are improved, reducing duplication
• Initial spend- with a financial save (return on money spent)
• Could create an income – if shared across more than one organsiation
• Speeding up benefit realisation
• Breaking down silos – CCIO can do this best
• Streamlining – cost savings and less wastage
• Will ensure meeting CQUIN targets (for example)
3. What are the clinical arguments for appointing a CCIO?
• Enabler for developing/improving clinical services
• Information systems will support clinical practice
• Minimises risk of clinicians disengaging
• Ensures clinical relevance
• Can better validate clinical info
• Coordination of clinical data capture
• Need clinical focus for design and configuration
• Closest to patients (capture and access)
• Understand complexity
o How care works
o How clinical information works
o How the business works
• Babel fish of healthcare
• Ability to multitask and manage a number of pieces of work
• Service improvement
• Ability to look at patients’ perspective
• Patient safety
• Risk management
• Clinical credibility – making information real
• Clinical management
• Clinician brings a different skill set to the team
• Increases the success rate of projects
• Ownership and drive
• Clinical process and understanding to change service models
• Needs to be clinically led
• Understanding patients’ needs ‘outcomes and benefits real time and wealth of info’
• Clinical expertise creates a credible challenge
• Helping to interpret ‘articulate’ the technical side
• Engagement = success
• Standardisation
• Improve safety
• Accountability
4. What is needed to make a compelling local business case for a CCIO?
• Health record tool – at the centre of patient care
• Information drives –
o Clinical quality
o Supports patients
o Improves decisions – clinical and business
o Facilitates safety
o Reduces cost
o Eliminates waste
o Supports planning
o Fuels research
• Ensure the EHR fits in with all clinical workflow
• Have a local champion
• Sign up at the senior level of organisations
• Good frontline engagement
• Clinical credibility
• Must do priority in organisation
• Commissioners specification
• Funding
• Benefits realisation
o Cost neutral
• Scenarios to support usefulness of the role
• Lessons learnt from organisations who have CCIOs
• Buy in from IT people
• Broad clinical engagement and credibility
• Identify the benefits to patients/staff/organisation – financial rewards
• Enhancing the ‘trust’ reputation