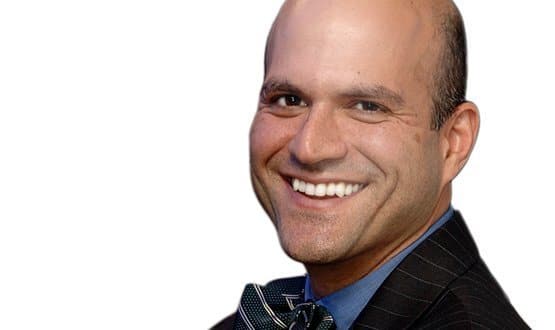
Dr Farzad Mostashari, US national health IT coordinator, says incentives tied to meaningful use standards have been ‘absolutely essential’ to the dramatic acceleration in its use of electronic health records.
With the NHS preparing guidance for a renewed push on electronic records and digitisation to increase safety and efficiency, the US experience shows that rapid progress is possible incentives and standards are clearly aligned.
NHS England is due to publish guidance for trusts in the first week of July on how they should use plan to use EPRs, as the first step towards health secretary Jeremy Hunt’s call for the NHS to become paperless by 2018.
EHI has been running The Big EPR Debate to collect ideas on what the guidance should focus on. The debate has uncovered reader backing for a roadmap for trusts at different stages of digital development, backed up by incentives for meaningful use.
Around two thirds of respondents to The Big EPR Survey supported the idea, with free text responses suggesting other readers were concerned about the potential for bureaucracy and gaming. As such, Dr Mostashari’s experience is revealing.
Defining the rules
The Obama administration launched a big push on EHRs as part of the American Reinvestment and Recovery Act, aiming to both kick-start the US economy and to control healthcare costs.
The 2009 Health Information Technology for Economic and Child Health (HITECH) Act was supported by meaningful use, for which there are two sets of ‘final rules’, with a third to follow.
Each set of rules is progressively more demanding than the last. The rules focus on how EHRs are used, rather than on the presence of systems.
Establishing these rules has generated huge debate and discussion within the US healthcare industry, in a lengthy process that has been pretty transparent and open.
Healthcare providers have to ‘attest’ to meeting the requirements to quality for payments. To get paid they must use an EHR system ‘certified’ to meet the requirements of the rules.
Broadly, the rules focus on the use of EHRs to capture and exchange standardised patient information; the use of EHRs to directly improve patient safety, through areas like closed loop medication systems; rigorous quality and outcomes reporting; enabling patient engagement; and providing the tools for population health management.
Four years of rapid growth
In 2008, a year before HITECH, just 9% of hospitals had adopted advanced EHRs, but by 2013, more than 80% had demonstrated meaningful use of EHRs. Of the $30 billion HITECH incentives $12.7 billion has so far been paid.
“I think meaningful use has been absolutely essential. To be able to change the conversation from ‘do you have a system, to what do you do with your system?” Dr Farzad Mostashari told EHI last month.
He said that one of the key aspects of setting out the rules of meaningful use was to change the dialogue, to move away from billing systems to areas like data exchange and population health management.
“In many ways it’s been essential to tip the axis of the industry; to flip the axis from focusing on documentation and billing machines, to tools that can help do population health management, can help provide safer care, and can encourage patient engagement and care co-ordination."
Meaningful use incentives provided the way to change priorities and get healthcare providers to demand new types of capability from their suppliers, he added.
“So it was a chicken and the egg problem and we’ve moved on both to simultaneously create both the payment context for more efficient, higher quality care as well as the tools needed to success in those context.”
Asked whether progress will continue after incentives end, Dr Mostashari is upbeat. “I think so. This was a good stimulus programme in that it primes the pump, it gets movement to occur and it creates a tipping point and an eco-system.”
He adds: “Once you’ve gone from 20% of hospitals having things like computerised physician order entry when medications are ordered, to 70% now and we’ll be up to 85-90% by next year. If that’s not a tipping point I don’t know what is.”
Getting to a tippng point
The US national health IT coordinator says that having achieved a critical mass of digitisation the data created is available to create new opportunities.
“The other tipping point is that data is oxygen for innovation in health ICT. So what we’ve created basically is enormous change in the digitalisation of healthcare encounters, and that information is now ripe for use to do analytics, predictive analytics, modeling, patient engagement tools that we never had before.”
He added that another good indicator is venture capital activity. “The amount of VC activity in health IT has doubled. So there are lots of indicators.”
Having passed the tipping point on data Dr Mostashari says that one of the most pressing challenges faced is to train healthcare professionals to make the most effective use of the data now available.
One of the key programmes funded by HITECH was in a network of 62 Regional Extension Centres to train healthcare staff in implementation of systems, support and guidance. Over $660m has been spent on the programme to date.
“Initially we focused a lot on implementation of health IT. What we are now realising is that the bigger need is to retrain existing healthcare workers on how to use data.
"Not necessarily implement systems, because that’s a short-term thing; what is forever is how you use data as part of your daily work, to constantly be improving.”
As a result of the big update in EHR systems, he added that the skills now at a premium in the digitised healthcare system are in areas like analytic skills, process re-engineering and change management.

EHI is running The Big EPR Debate to give readers a chance to shape the future of electronic records and a paperless NHS. What should NHS England’s guidance cover? What is an EPR? What is essential and what can be left for later? What should the next steps be. Join the debate.