The Personalised Care Institute (PCI) has launched virtual reality training on shared decision-making for healthcare professionals to help plug the gaps professionals report in their knowledge.
Commissioned by NHS England, the PCI training will explore the key micro-skills around shared decision-making of agenda setting, teach-back, exploring patient preferences around treatment options and reaching a shared decision. By practising these skills in a risk-free environment, staff will be able to improve and develop their skills for the benefit of their patients.
Shared decision-making (SDM) has been found to result in better patient outcomes, with increased adherence to treatment, reduced repeat appointments and few regrets about decisions made over their health and care.
Yet, according to The Patient Association, 46% of healthcare professionals report gaps in their knowledge on the topic, and 70% say they would like to learn more.
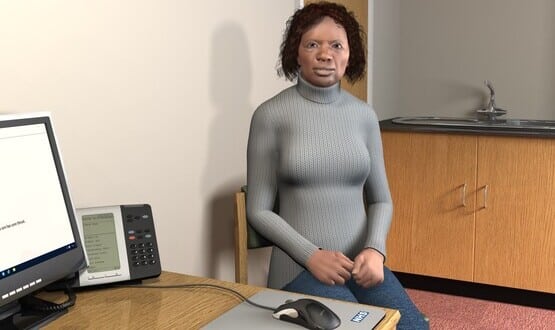
Virtual Patient Simulation: Test Your Personalised Care Conversations has been developed by PCI in conjunction with Keele University. The free, quality-assured eLearning tool allows users to put their shared decision-making skills to the test through a series of life-like simulated patient consultations.
It uses multiple choice questions to provide a structured interaction with an on-screen animated patient character. Comprehensive feedback is delivered at the end of each exercise, allowing users to put what they’re learning to the test with repeated use.
Dr Emma Hyde, clinical director of the PCI, said: “While research suggests that, currently, only one in three HCPs always practise SDM fully, the fact that perceived common barriers include lack of experience, confidence and time suggests that these could be quickly overcome with the opportunity to practise.”
She continued: “Not only will this training, commissioned by NHSE, equip health and care professionals with the shared decision-making skills and knowledge needed to deliver the very best health outcomes for patients, it will also address the growing desire amongst the general public for greater involvement in key decisions that inform their healthcare.”
Simulations encouraging engagement
The use of simulations can help to encourage greater engagement and facilitate repetitive practise, and at the same time allows users to work at their own pace.
Dr Priti Kadoo, a GP in frailty medicine and an ambassador for the PCI, said: “It helps you to reflect on current practice and really think about personalised care and striking the right balance between imparting clinical information while considering how the patient feels and is likely to respond to what you tell or ask them. It is a great way to learn and I enjoyed using it.”
The first scenarios to be launched are an in-person consultation based on an osteoarthritis discussion and a remote consultation by telephone with a father concerning his son’s sore throat. Two further scenarios – a referral for suspected bowel cancer and a discussion around the ongoing use of antidepressants – are due to be launched in the coming months.
The use of VR to train healthcare professionals is becoming more widespread. Last year Norfolk and Norwich University Hospitals NHS Foundation Trust introduced new virtual reality films for dementia education. The aim of the VR films was to help healthcare professionals gain a better understanding of the challenges patients living with dementia face when on a busy inpatient ward.