An influential US safety expert, called in to advise the government on creating a ‘zero harm’ NHS in the wake of the Mid Staffordshire scandal, has called for “complete transparency of data.”
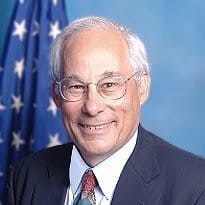
Professor Don Berwick, a former health advisor to US president Barack Obama, delivered a report to the UK government this morning in which he urged NHS organisations to publish all the data they had available on quality and safety.
“Transparency should be complete, timely and unequivocal,” it says. “All non-personal data on quality and safety, whether assembled by government, organisations, or professional societies, should be shared in a timely fashion with all parties who want it, including, in accessible form, with the public.”
The report – ‘A promise to learn – a commitment to act: improving the safety of patients in England’ – adds that patient safety cannot be improved without “active interrogation of information.”
“Information should include: the perspective of patients and their families; measures of harm; measures of the reliability of critical safety processes; information on practices that encourage the monitoring of safety on a day to day basis; on the capacity to anticipate safety problems; and on the capacity to respond and learn from safety information,” it says.
Professor Berwick is the former head of the Institute for Healthcare Improvement, which has led work on encouraging healthcare systems worldwide to create a culture of safety by learning from other sectors, such as aviation.
He was asked to conduct a review of safety in the NHS by Prime Minister David Cameron following the publication of the second of Robert Francis QC’s reports into Mid Staffordshire NHS Foundation Trust, where patients suffered very poor care in the A&E department and some wards.
Health secretary Jeremy Hunt was present at the publication of today’s report. But the government has said that it will respond to its recommendations and the Francis inquiry’s recommendations in “the autumn.”
Some responses, such as a shake-up of the CQC’s inspection regime, the introduction of ‘Ofsted-style’ ratings for trusts and departments, and a new measure of ‘avoidable harm’ have already been announced.
The last development is being led by NHS England chief medical officer Sir Bruce Keogh, in response to scepticism about the construction and use of the most widely used mortality ratios in the NHS, the HSMR and SHMI.
The Berwick report picks up on this by saying there is no single measure for safety. It also says the NHS should use mortality indicators as a “smoke alarm”, but not to rate hospitals.
“There is no single measure of safety, but early warning signals can be valuable and should be maintained and heeded,” it says.
However, the report warns that NHS organisations often do not have the capacity to analyse the data they have available.
“Most health care organisations at present have very little capacity to analyse, monitor, or learn from safety and quality information. This gap is costly, and should be closed,” says the report.
“Commissioners should increase funding for NHS organisations to analyse and effectively use safety and quality information.”
As well as highlighting the need for transparency, the report says that patients and carers need to be involved and heard all the way from ward to board level.
“We really urge you to get serious about listening to patients,” Professor Berwick told a report launch this morning. “The same goes for staff; listening to them is key. Anything that restricts a staff member to speak up about a safety issue should not be there.”
Other areas for action identified by the report include: reducing patient harm by embracing an ethic of learning; leadership; ensuring adequate staffing; training and capacity building; making supervisory and regulatory systems simple and clear; and introducing criminal sanctions as a deterrent to wilful or reckless neglect or mistreatment.
Health secretary Jeremy Hunt said: “This is a strong endorsement of all that the government has delivered since the Francis report, including on transparency, putting patients first, duty of candour and CQC reform,” he said.
“For too long, patient safety and compassionate care have been secondary concerns in parts of the NHS and this has to change.”